More Information
Submitted: August 06, 2021 | Approved: December 30, 2021 | Published: December 31, 2021
How to cite this article: Mythili G, Selvarani E, Marcelin Ancy R. A comparitive study on square stepping exercise versus balance training exercises on fear of fall and balance in parkinsonism patients. J Nov Physiother Rehabil. 2021; 5: 027-031.
DOI: 10.29328/journal.jnpr.1001042
Copyright License: © 2021 Mythili G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Parkinsonism patient; Balance; Square stepping exercise training; Balance training exercise
A comparitive study on square stepping exercise versus balance training exercises on fear of fall and balance in parkinsonism patients
Mythili G1, Selvarani E2 and Marcelin Ancy R1*
1Department of Physiotherapy and Rehabilitation Centre Faculty of Physiotherapy, Cherraan’s Institute of Health Science, Coimbatore, India
2Department of Physiotherapy and Rehabilitation Centre, Principal, Cherraan’s Institute of Health Science, Coimbatore, India
*Address for Correspondence: Marcelin Ancy R, Department of Physiotherapy and Rehabilitation Centre Faculty of Physiotherapy, Cherraan’s Institute of Health Science, Coimbatore, India, Email: [email protected]
To study the effect of square stepping exercise and balance exercise to improve balance impairment and reducing the fear of falling on Parkinsonism patient. This is a pre-test and post-test experimental design comparative in nature. Subject aged between 60 – 70 years having Parkinson’s disease were included for the study. Group A (15 subjects) participated in square stepping exercise for 5 times in a week for 4 weeks and Group B (15 subjects) participated in balance exercise for 5 times in a week for 4 weeks. The outcome was measured by using Berg balance scale, Time up and go (TUG) test and fall efficacy scale. Statistical analysis done by using pair ‘t’ test and unpair ‘t’ test showed that there is significant improvement in subject who underwent the square stepping exercise program compared to balance exercise on fear of fall and balance in parkinsonism patients. It is concluded that square stepping exercise group exhibited statistically significant improvement in Berg Balance Scale, Time up and Go test score and fall efficacy test score compared to the balance training exercise group.
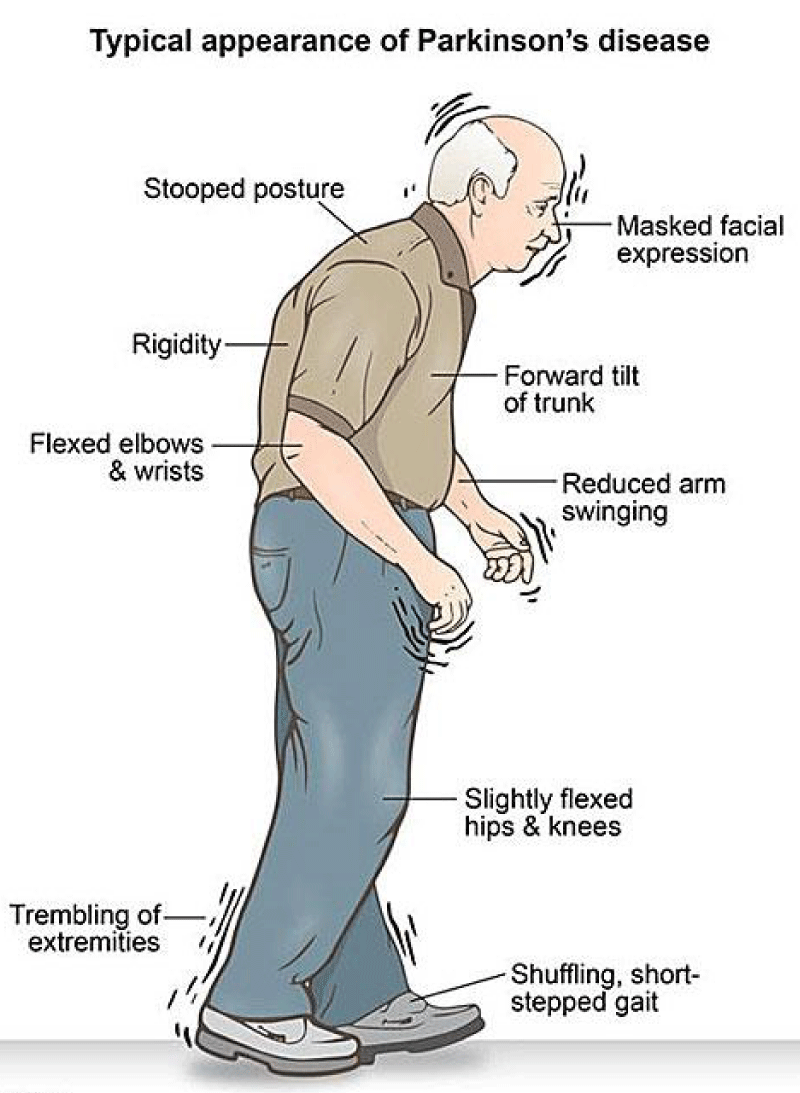
Parkinson’s disease is a neurodegenerative disorder affecting people throughout the world. It is estimated that 10 million people suffer from Parkinson’s disease worldwide. The WHO suggested an “estimated crude prevalence” (the total number of existent cases of Parkinsonism patients each year, old, and new) of 160/100,000, and an estimated incidence (the number of new cases each year) of 16–19/100,000. Epidemiological study of Parkinson’s disease has been better studied than any other disorders in India. Patients with Parkinson’s disease typically show prominent locomotion problems such as shuffling gait, stooped posture, impaired balance, and freezing of gait. Freezing of gait also is one of the most common devitalizing aspects of Parkinson’s disease and has been linked to injuries, falls, and reduced quality of life. Gait and balance problem in Parkinson’s disease will leads to increased disability and decreased health‑related quality of life and survival. Improving gait and balance and thus preventing falls are notoriously difficult to treat and responds poorly to pharmacological or surgical treatment, and is, therefore, a major therapeutic challenge in Parkinson’s disease. Parkinson’s disease Patients who participated in balance training exercises have shown significant improvements in their gait and ambulation.
Patients who undergone physio therapy consisting of strength exercises, balance, and gait training in addition to medication therapy show short‑ and long‑term increases in quality of life, gait pattern, walking speed, cadence and activities of daily living when compared to patients who only received medication. Physical exercises that include a balance component can reduce the fear of fall and improve gait among Parkinson’s disease patients. For the effective, balance training exercise therapist should be undertaken with reduced base of support, minimized upper limb support, and include weight shifting components such as stepping. Most rehabilitation studies in Parkinson’s disease suggest the treatment of bradykinesia and effect of balance rehabilitation on fear of fall and balance. Recent systematic reviews concluded that evidence available was insufficient to support the efficacy of physiotherapy in Parkinson’s disease or to support the use of one form of physiotherapy over another. Therefore, the development of rehabilitation approaches that work along with current treatment is important to manage these balance problems.
Balance is a complex multi system process involving the reception and integration of sensory inputs and the planning and implementation of movement to achieve a goal requiring upright erect posture. Every activity we carry out requires us to react against gravity & our body to adjust accordingly in order to maintain optimal balance. Balance is not an independent quality, but underlies our capacity to do a wide range of activities that constitute normal daily life. Activities such as sitting in an armchair, carrying a struggling child, cleaning a high window or running across a busy road require different and complex changes in muscle tone and activity within the balance control system. Balance cannot be separated from the action of which it is an integral component, or from the environment in which it is performed.
Balance therefore forms the “foundation for all voluntary motor skills”. Normal balance requires control of both gravitational forces to maintain posture and acceleration forces to maintain equilibrium. Together, the postural and equilibrium components of balance control ensure stability of the body during widely differing activities. It is the ability to control centre of gravity (COG) over the base of support in a given sensory environment. According to the dynamic systems model, balance is the result of interactions between the individual, the task the individual is performing, and the environment in which the task must be `performed.
Study design: A pre-test and post-test experimental design comparative in nature.
Study setting: The study was conducted in Department of Physiotherapy and Rehabilitation Centre, principal, Cherraan’s institute of health science, Coimbatore.
Study duration: The study was conducted for a period of 6 months.
Treatment duration: The treatment duration is that exercise program was given 5 times in a week for 4 weeks.
Population and sampling: 30 subjects were selected by convenient Sampling method.
Inclusion criteria
- Age more than 60 years.
- Parkinsonism disease.
- Hoehn- yahr scale stage of II and III abilities to walk without any physical assistance.
- Mini- mental Examination score > 26.
Exclusion criteria
- Musculoskeletal condition like joint replacement, fracture, etc.,
- Cardiopulmonary condition
- Any other Neurological condition other than parkin-sonism disease
- Patient diagnosed with visual and auditory impairment.
- Uncontrolled diabetes mellitus
Materials used
- Mat (2.5 m × 1.0 m) 40 small square of 25 cm each.
- Stepper
- ball
- balance beam
Parameter for analysis
- Berg Balance Scale
- Time up and Go Test
- Fall efficacy scale
Procedure
The subjects for the study are Parkinsonism patient’s age above 60 year who have balance impairment and fear of falling. After explaining about the study procedure and informed consent was obtained. Then the subjects were assigned to Group A (15) and Group B (15) by randomized allocation method. Retest assessment of balance and fear of falling was done using berg balance scale, time up and go test and fall efficacy scale. Intervention is divided into three parts. Warm up, group intervention, and cool down. Warm up and cool down are same for both groups. Warm up: Participants started with muscle stretches for the upper limb and lower limb followed by joint movements being performed in all planes.
For Group A, the exercise training is based on the usage of a “floor mat” (2.5 m × 1.0 m), partitioned into 40 small squares of 25 cm each square. Basic Elementary pattern 1 and 2 were used in this study. Participants were given instruction to walk (step) in step pattern from one end of the mat to the other. They were asked to return to their starting position by walking normally off the mat, when the participant reached the end of the mat and they start next stepping pattern. Each participant repeated each sequence pattern three times and then started a new pattern. Sequences of walking pattern were forward, backward, lateral, and oblique steps, and for each sequence pattern, the complexity of the steps combination was set higher. This intervention was applied five times a week, for 4 weeks and it is followed by cool down exercises for 5 minutes.
For Group B, In Balance exercise training a circuit of static and dynamic balance exercise was given by reducing the base of support (bipedal to tandem), moving from even to uneven base of support, providing external challenges to balance that require a reaction, narrowing the base of support while responding to the external challenge and increasing the difficulty of tasks (e.g., changing direction, changing speed, walking with reduced base of support, turning, bending, stepping on and off curbs, braiding/ grapevine steps, walking while carrying a objects, or clearing the obstacles). Functional ankle, knee and hip strengthening exercises which includes heel and toe rises and rising from a chair, followed by cool down exercise for 5 minutes. Cool down: The rhythm becomes slower. Relaxation exercises include slow walking, swinging legs in standing, stretching lower limbs and trunk. After 4 weeks post-test assessment was taken.
Statistical methods
Data analysis is the method of evaluation in the research study. In this study evaluation the data is through the descriptive statistical methods.
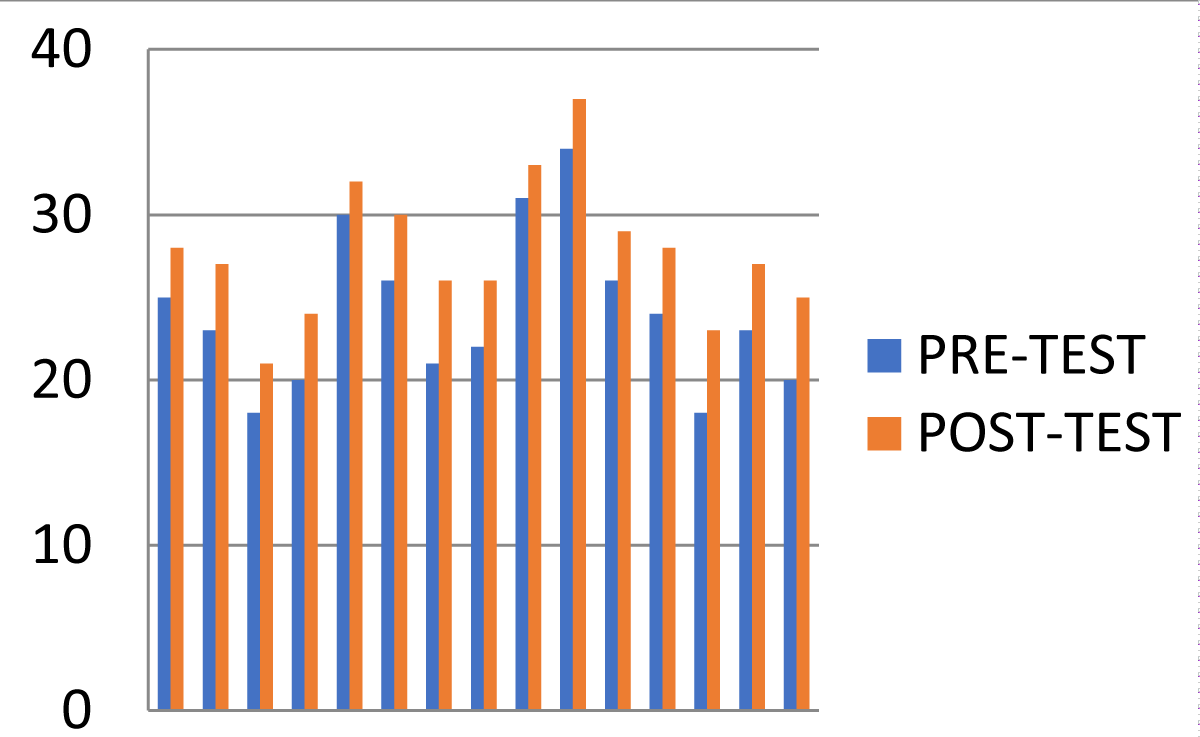
| Group | Test | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| A | Pre-test Post-test |
23.06 28.8 |
5.53 | 1.06 | 20.2 | 3.326 |
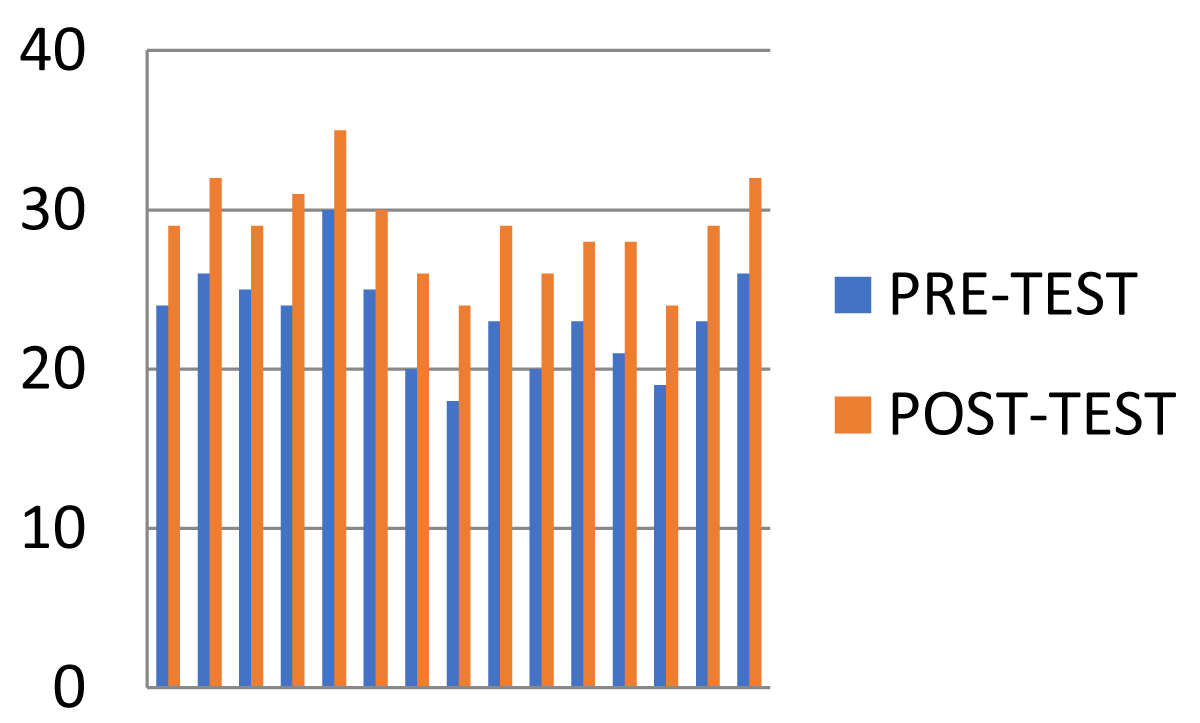
Comparison between pre- and post-test (berg balance scale) values of Group A.
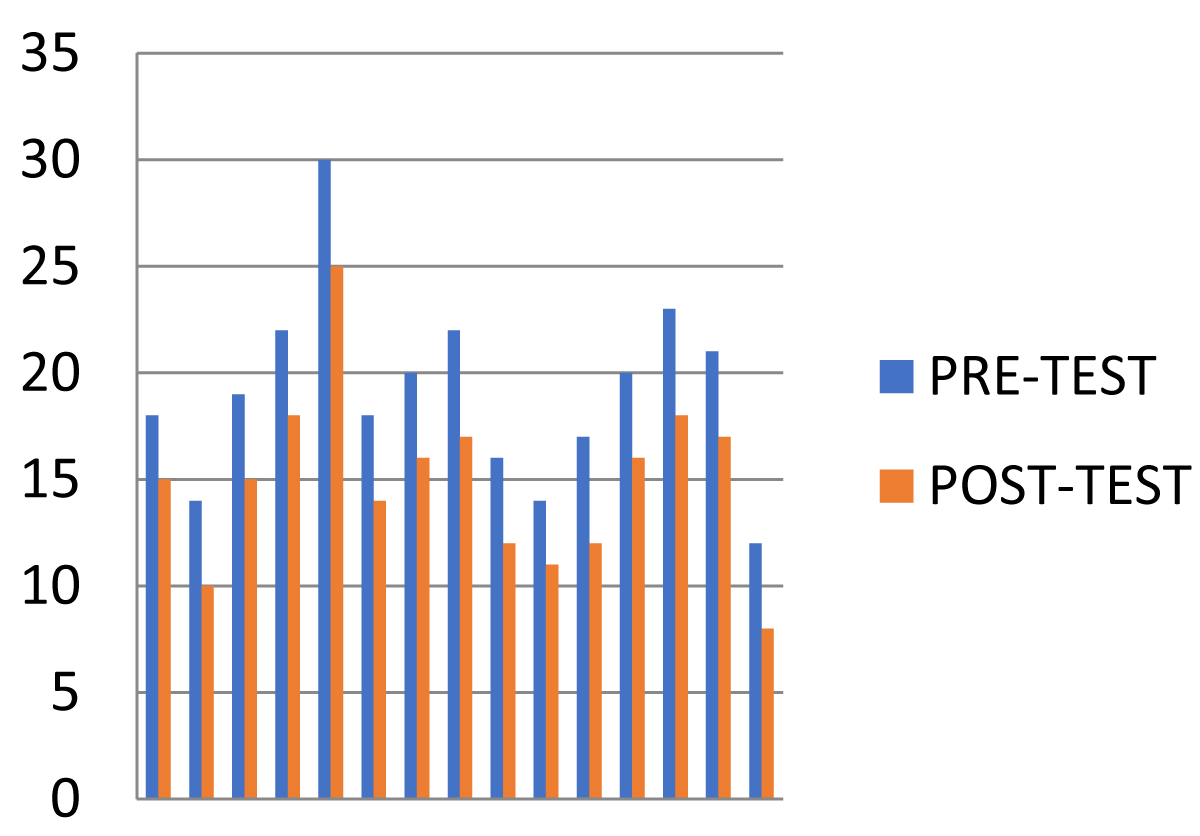
| Group | Test | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| A | Pre-test Post-test |
17.4 12.86 |
4.83 | 0.9904 | 17.714 | 3.326 |
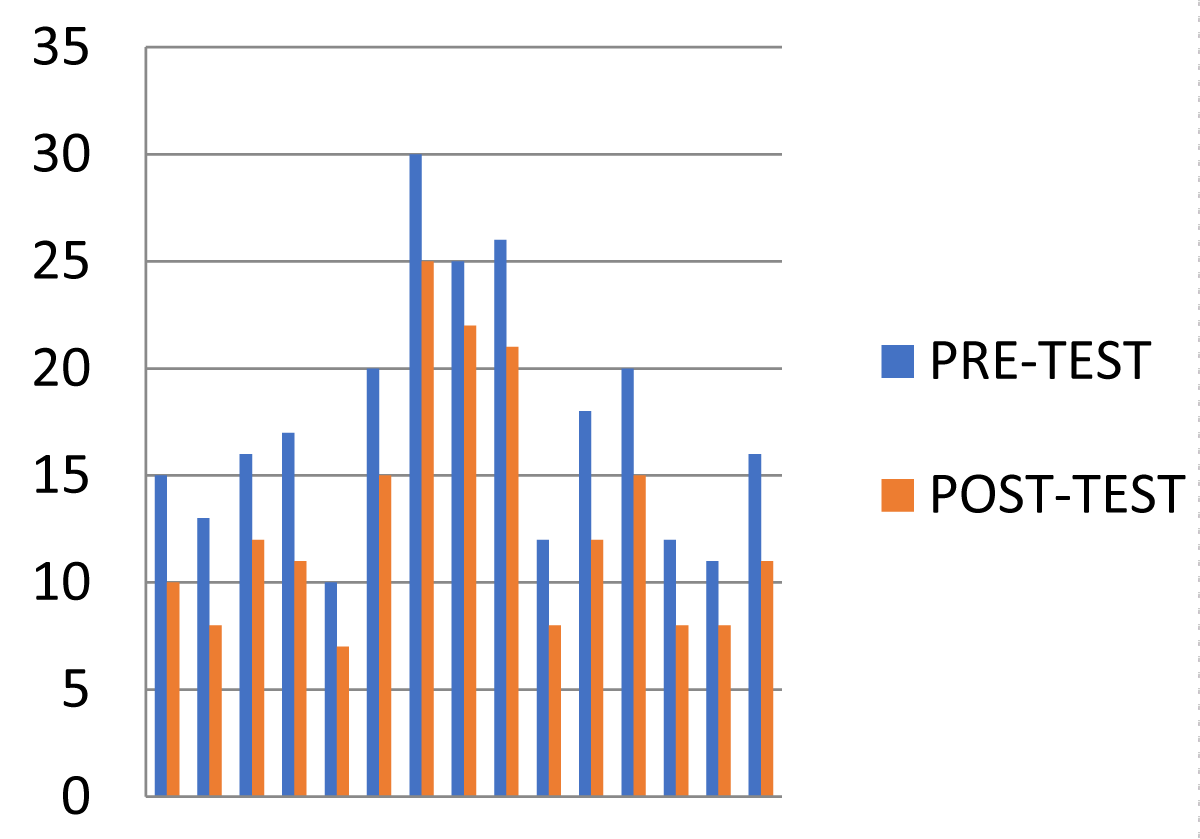
Comparison between pre- and post-test (time up and go test) values of Group A.
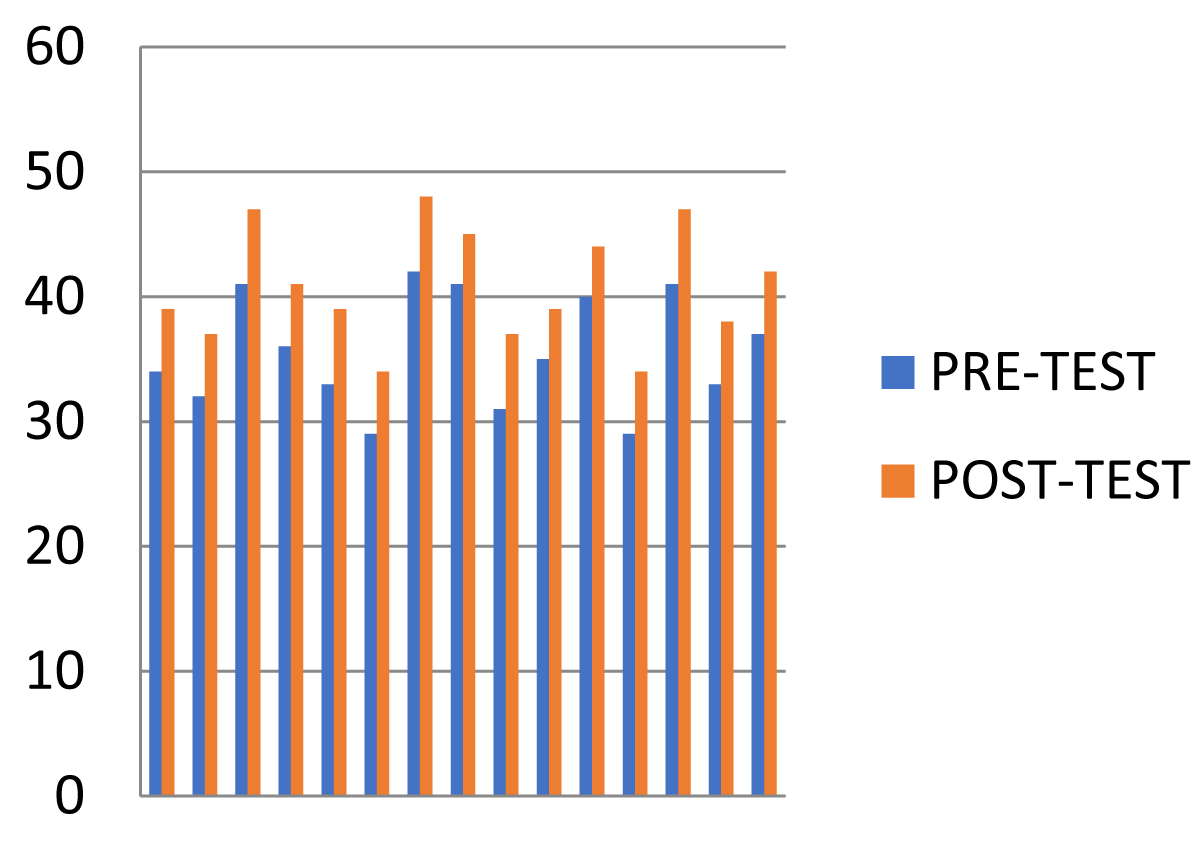
| Group | Test | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| A | Pre-test Post-test |
30.33 37.77 |
7.44 | 0.98 | 29.07 | 3.326 |
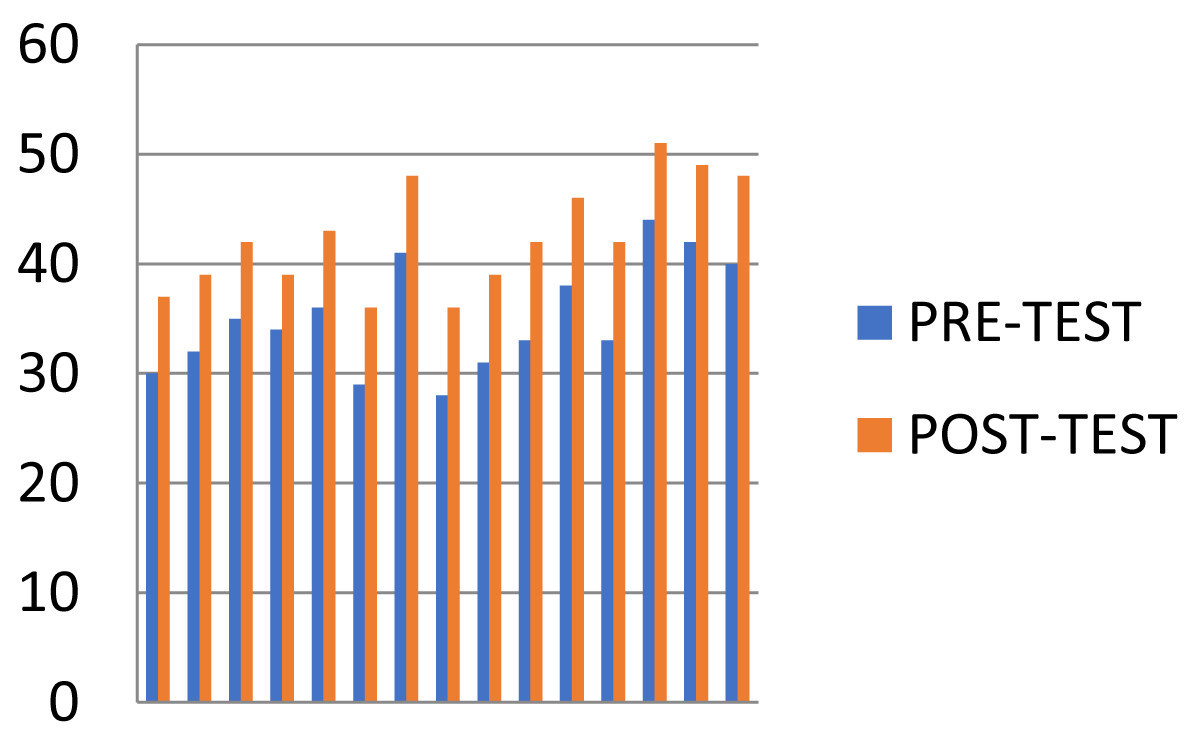
Comparison between pre- and post-test (fall efficacy scale) values of Group A.
| Group | Test | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| B | Pre-test Post-test |
24.06 27.73 |
3.66 | 0.975 | 14.52 | 3.326 |
Comparison between pre- and post-test (berg balance scale) values of Group B.
| Group | Test | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| B | Pre-test Post-test |
19.0 14.93 |
4.266 | 0.98 | 16.7582 | 3.326 |
Comparison between pre- and post-test (time up and go test) values of Group B.
| Group | Measurement | Mean | Mean difference | SD | Paired ‘t’ test | ‘t’ table value at 0.005 |
| B | Pre-test Post-test |
35.60 40.73 |
5.13 | 0.7432 | 20.1581 | 3.326 |
Comparison between pre- and post-test (fall efficacy scale) values of Group B.
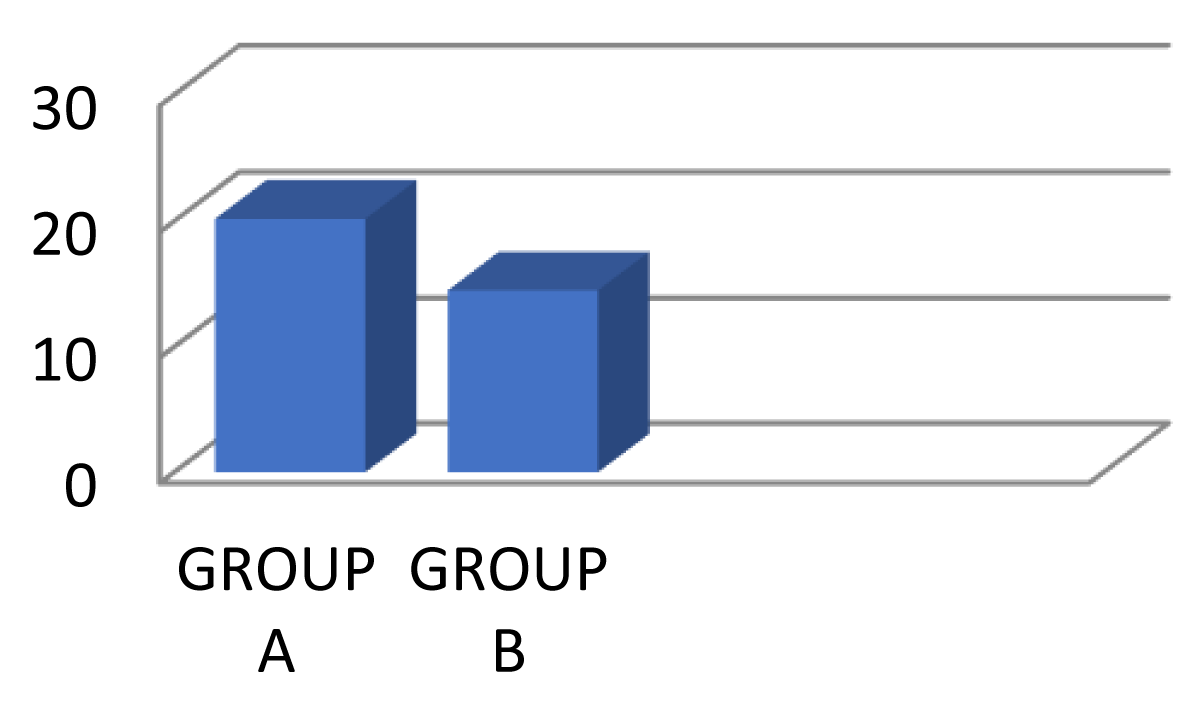
| Group | ‘t’ value | ‘t’ value Difference |
SD | Unpaired ‘t’ test | ‘t’ table value at 0.005 |
| A B |
20.20309 14.524 |
5.67909 | 1.01886 | 5.02688 | 3.047 |
Comparison between post-test (berg balance scale) values of Group A and B.
| Group | ‘t’ value | ‘t’ value Difference |
SD | Unpaired ‘t’ test | ‘t’ table value at 0.005 |
| A B |
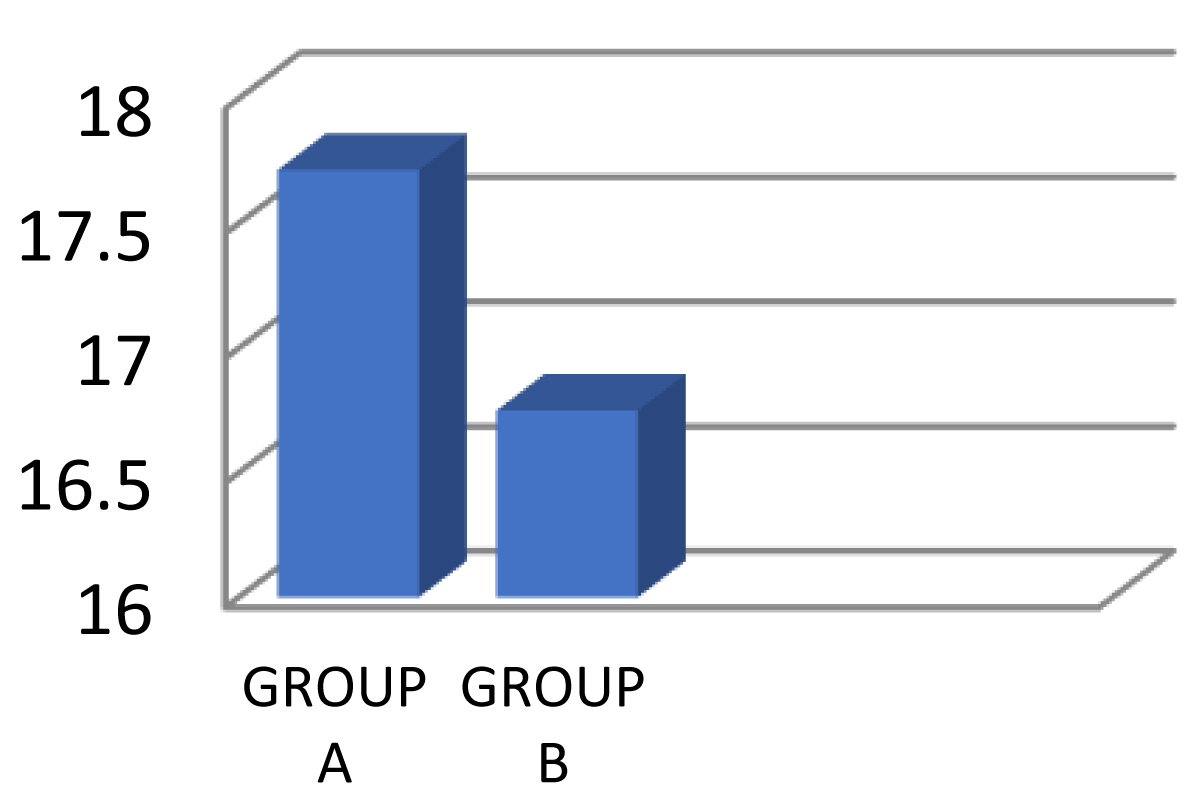
17.71 16.752 |
0.9622 | 0.98745 | 1.58109 | 3.047 |
Comparison between post-test (time up and go test) values of Group A and B.
| Group | ‘t’ value | ‘t’ value Difference |
SD | Unpaired ‘t’ test | ‘t’ table value at 0.005 |
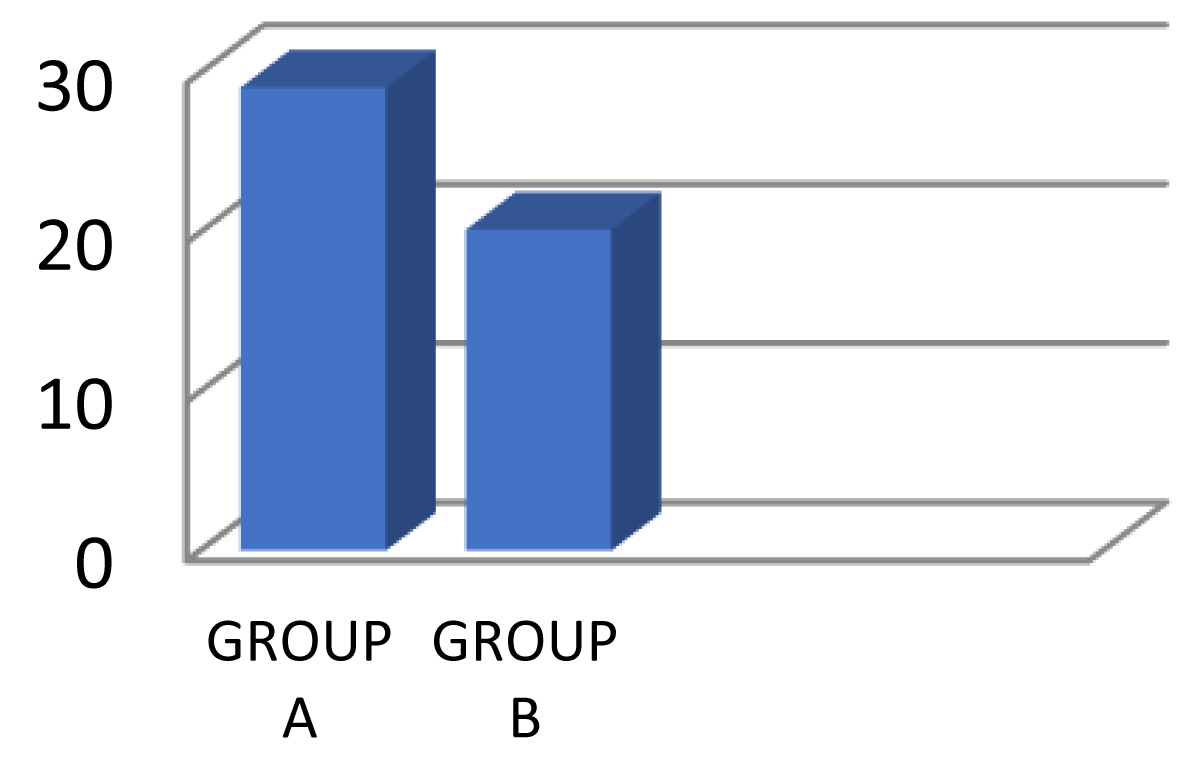
| A B |
29.078 20.1581 |
8.92 | 0.8728 | 7.1238 | 3.047 |
Comparison between post-test (fall efficacy scale) values of Group A and B.
Hariharasudhan Ravichandran and Balamurugan Janaki Raman, stated that Square stepping exercise is more effective in improving balance and gait in Parkinson’s disease patients. Further studies with larger population are needed, the result of this study shows that SSE could be used as a mean of rehabilitation in Parkinson’s disease patients. Jessica Rodrigues Pereira and Sebastião Gobbi explained the effects of Square-Stepping Exercise (SSE) on symptoms of balance and functional locomotion in older population. Participants were divided into two groups: Trained Group (TG), who performed a 16-week intervention with square stepping exercise and Control Group (CG), who performed only evaluations. The Berg Balance Scale and Time Up and Go Test (TUG) constituted the evaluation protocol to verify balance and functional locomotion. Geriatric Depression Scale-short form (GDS-15) was applied for measure depressive symptoms. Evaluations were realized pre and post 16-week. Significant changes were seen in the trained group with the maintenance of GDS-15 scores and on the time to perform the TUG test which reflects better functional locomotion than the control group. Thus, the study concludes that the square stepping exercise is an important tool for improving the balance impairment, prevent fear of falls and decrease depression symptoms. Teixeira CV1, Gobbi S, Pereira JR, Vital TM, Hernandéz SS, Shigematsu R and Gobbi LT [1] conclude that square stepping exercise group showed a significant improvement in cognitive improvement, concentrated attention and mental flexibility of the individual after 16 weeks of the square stepping exercise. Results shows that square stepping exercise gives positive improvement in cognitive functions in older population. Shigematsu and Okura T [2] analysed that the square stepping exercise shows significant improvements in agility, leg power, locomotion speed, flexibility and balance. No significant changes were detected in any outcome tool in the control group. The square stepping exercise improved lower limb functional capacities, lack of which constitutes a fear of falls in the elderly. This exercise program should be further studied to know its effectiveness to reduce the fear of falls in the older population.
Group A: The result showed that, the exercise group who performed square stepping exercise among parkinsonism patient with reference to group A (berg balance scale) ‘t’ calculated value (20.2) is significantly greater than 3.326 (p > 0.05). For (Time up and go test) ‘t’ calculated value (17.714) is significantly greater than 3.326 (p > 0.05). For (Fall efficacy scale) ‘t’ calculated value (29.07) is significantly greater than 3.326 (p > 0.05). Hence alternative hypothesis (H1) is accepted.
Group B: The result showed that, the exercise group who performed square stepping exercise among parkinsonism patient with reference to group A (berg balance scale) ‘t’ calculated value (14.52) is significantly greater than 3.326 (p > 0.05). For (Time up and go test) ‘t’ calculated value (16.7582) is significantly greater than 3.326 (p > 0.05). For (Fall efficacy scale) ‘t’ calculated value (20.1581) is significantly greater than 3.326 (p > 0.05). Hence alternative hypothesis (H1) is accepted.
On comparing groupa and group B: When comparing both group values by a paired (Berg balance scale) ‘t’ test the calculated ‘t’ value is (5.02688) and ‘t’ table value (3.047) > 0.05. For (Time up and go test) ‘t’ test the calculated value (1.5810) and ‘t’ table value (3.04) > 0.05. For (fall efficacy scale) ‘t’ test calculated value (7.1238) and ‘t’ table value (3.047) > 0.05. Hence unpaired ‘t’ test shows comparative effects of group A and group B. Hence, we conclude that, square stepping exercise is more effective than the balance exercise in improving balance and reducing fear of fall in Parkinsonism patients.
From the data presentation and analysis, it is evident that: In the study we conclude that the parkinsonism patient who underwent square stepping exercise are more effective than patient who underwent balance exercise in improving the balance and reducing the fear of fall among the parkinsonism patients.
The authors would like to thank all the students who participated in the study.
Ethical Approval: Approved
- Cynthiyanorkin PT. Biomechanics, 3rd edition 2004.
- Kisner C, Colby LA. Therapeutic exercise foundation and technique, 6th edition, 2013.
- Tinetti ME, Speechley M, Ginter SF. Risk factors for fall among elderly persons living in the community. N Engl J Med. 1988; 319: 1701-1707. PubMed: https://pubmed.ncbi.nlm.nih.gov/3205267/
- Mancini M, Nutt JG, Horak FB. Balance dysfunction in Parkinson’s disease.
- William Smith MS. The complete fitness guide to improve mobility, strength and Balance exercise for Parkinson’s Disease.
- Incidence, Prevalence and Cost of Parkinson's disease. 2011. http://www.eng.ircminternational.com/2011/04/incidence-prevalence-and-cost-of- Parkinson’s-disease/
- Ellis T, de Goede CJ, Feldman RG, Wolters EC, Kwakkel G, et al. Efficacy of a physical therapy program in patients with Parkinson's disease: A randomized controlled trial. Arch Phys Med Rehab. 2005; 86: 626-632. PubMed: https://pubmed.ncbi.nlm.nih.gov/15827910/
- Heremans E, Nieuwboer A, Spildooren J, Vandenbossche J, Deroost N, et al. Cognitive aspects of freezing of gait in Parkinson's disease: A challenge for rehabilitation. J Neural Transm (Vienna). 2013; 120: 543-557. PubMed: https://pubmed.ncbi.nlm.nih.gov/23328947/
- van der Kolk NM, King LA. Effects of exercise on mobility in people with Parkinson's disease. Mov Disorder. 2013; 28: 1587-1596. PubMed: https://pubmed.ncbi.nlm.nih.gov/24132847/
- Özgönenel L, Çagirici S, Çabalar M, Durmusoglu G. Use of game console for rehabilitation of Parkinson'sdisease. Balkan Med J. 2016; 33: 396-400. PubMed: https://pubmed.ncbi.nlm.nih.gov/27606134/
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, et al. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J Am Geriatric Soc. 2008; 56: 2234-2243. PubMed: https://pubmed.ncbi.nlm.nih.gov/19093923/
- Nieuwboer A, Kwakkel G, Rochester L, Jones D, van Wegen E, et al. Cueing training in the home improves gait-related mobility in Parkinson's disease: The RESCUE trial. J Neurosurg Psychiatry. 2007; 78: 134-410. PubMed: https://pubmed.ncbi.nlm.nih.gov/17229744/
- Shigematsu R, Okura T. A novel exercise for improving lower-extremity functional fitness in the elderly. Aging Clin Experie Res. 2006; 18: 242-248. PubMed: https://pubmed.ncbi.nlm.nih.gov/16804371/
- Hoehn MM, Yahr MD. Parkinsonism: Onset, progression and mortality. Neurology. 1967; 17: 427-442. PubMed: https://pubmed.ncbi.nlm.nih.gov/6067254/
- Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: Validation of an instrument. Can J Public Health. 1992; 83: S7-11. PubMed: https://pubmed.ncbi.nlm.nih.gov/1468055/
- Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39: 142-148. PubMed: https://pubmed.ncbi.nlm.nih.gov/1991946/
- Harshika B, Vishnu V, Tushar P, Shilpa K. Comparative study on the effect of square stepping exercises versus balance training exercises on fear of fall and balance in elderly population. Int J Physiother Res. 2016; 4: 1352-1359.
- Smania N, Corato E, Tinazzi M, Stanzani C, Fiaschi A, et al. Effect of balance training on postural instability in patients with idiopathic Parkinson's disease. Neuro Rehab Neural Repair. 2010; 24: 826-834. PubMed: https://pubmed.ncbi.nlm.nih.gov/21045119/
- Rochester L, Baker K, Hetherington V, Jones D, Willems AM, et al. Evidence for motor learning in Parkinson's disease: Acquisition, automaticity and retention of cued gait performance after training with external rhythmical cues. Brain Res. 2010; 1319: 103-111. PubMed: https://pubmed.ncbi.nlm.nih.gov/20064492/
- Teixeira CV, Gobbi S, Pereira JR, Vital TM, Hernandéz SS, et al. Effects of square-stepping exercise on cognitive functions of older people. Psychogeriatrics. 2013; 13: 148-156. PubMed: https://pubmed.ncbi.nlm.nih.gov/25913763/