More Information
Submitted: June 25, 2022 | Approved: October 17, 2022 | Published: October 18, 2022
How to cite this article: Bellomo RG, Barbato C, Porreca A, Saggini R. Rehabilitation protocol with VISS system and human synergy mat in subjects with flat foot problems in developmental age. J Nov Physiother Rehabil. 2022; 6: 018-022.
DOI: 10.29328/journal.jnpr.1001046
Copyright License: © 2022 Bellomo RG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Rehabilitation protocol with VISS system and human synergy mat in subjects with flat foot problems in developmental age
Rosa Grazia Bellomo1, Claudia Barbato1* , Annamaria Porreca2 and Raoul Saggini3
, Annamaria Porreca2 and Raoul Saggini3
1Department of Biomolecular Sciences, University of Study of Urbino Carlo Bo, Urbino, Italy
2Department of Economics, ‘Gabriele d’Annunzio’ University, Chieti-Pescara, Italy
3Department of Medicine and Aging Sciences Gabriele d’Annunzio’ University, Chieti-Pescara, Italy
*Address for Correspondence: Claudia Barbato, Department of Biomolecular Sciences, University of Study of Urbino Carlo Bo, Urbino, Italy, Email: [email protected]
The flat foot can be defined as a syndrome with multiple etiopathogenesis, characterized by an altered structure of the longitudinal arch of the plantar vault with its reduction in height. The plantar arch collapse can be counteracted by strengthening the muscles involved; for many years, specific physical exercises have been proposed for this purpose in physical and rehabilitation medicine. Our work aimed to improve the plantar arch muscles’ tone using high focal vibration therapy (300 Hz).
Methods: 49 children with a 3rd degree flat foot (age: 8,7,6) underwent 10 sessions, 2 days/wk, of 30 min of focused high vibratory therapy at a frequency of 300 Hz (Vissman, Italy). Before and after treatment stabilometry (StT), static and dynamic baropodometry tests were performed.
Results: Evaluation of StT showed an improvement in stability and a decrease in the sway area and ellipse area. Baropodometry tests showed a decrease in foot surface. Also, dynamic tests showed a decrease in both foot surfaces.
Discussion: The results lead us to consider this method as a method of the first choice for a conservative approach in the rehabilitation of flat foot syndrome and also for 3rd grade children [1,2].
Flatfoot is a common syndrome with multiple etio-pathogenesis, that has long been associated with pain and disability, and very often worries parents for their children’s health and mobility. The generic term “flatfoot” describe any condition in which the longitudinal foot arch is abnormally low or absent [3]. It is characterized by an altered structure of the longitudinal arch of the plantar vault with its reduction in height and by heel eversion and talar prominence.
The flat foot is characterized by medial rotation and plantar flexion of the talus, heel eversion, sagging of the medial arch and adduction of the forefoot. Harris and Beath scholars have divided flat feet into three categories: [2,4-6].
Flexible flat foot
The longitudinal arch of the foot collapses during the cushioning of the body weight to then restore itself after the removal of the same, most flat flexible feet are physiological, asymptomatic and do not require treatment [6,7].
Rigid flat foot
Flattened rigid arch both in the body weight cushioning phase and in the “resting” phase. Flat foot with shortening of the Achilles tendon.
At birth, everyone has flat feet. In early infancy, the foot is mostly characterized by subcutaneous fat, the muscles are weak and the ligaments are still lax this leads to a physiological deviation of the calcaneus towards the outside. After several years (5/6) we are witnessing a progression of the rear foot that moves inwards and has a development of the arch of the foot [7-9].
The flat foot in pediatric age is commonly found so much to be considered in most cases a variable of the normal conformation of the child’s foot, in fact about 90% of children under 2 years of age have a more or less pronounced flattening of the plantar vault which is spontaneously reduced by 4% after 10 years of age with the normal physiological growth of the musculoskeletal system.
A 2006 study of 835 children between 3 and 6 years showed that the influence of flat feet is influenced by three factors [8-10] (age, gender, and weight) and manifests itself with a greater prevalence on younger, male subjects and overweight.
We hypothesized that postural control would improve after this treatment; in fact, somatosensory input from the lower limb has long been recognized as an important source of sensory information in controlling standing balance (Allum, et al. 1998), and several pieces of evidence suggest a contributing role of cutaneous receptors from the foot in controlling standing balance (Kennedy, et al. 2002).
Moreover, Maurer and coil. Demonstrated that mechanical stimulation of the plantar skin during quiet stance evokes postural sway that is highly correlated with the cutaneous stimuli (Maurer, et al. 2001). Foot sole presents a characteristic distribution of cutaneous receptors, and it was analyzed by Perry and coli (2000), Trussol (2001), and Kennedy and coil (2002). They demonstrated that the distribution of the receptors was preferential in the anterior lateral border and heel on the foot, that corresponds to the critical regions that take up the majority of the body’s weight are loaded conditions (Perry, et al. 2000). They also observed that a large percentage of the skin receptors are fast adapting (FA) and have an elevated activation threshold (if compared with the glabrous skin of the hand).
The working group is composed of 49 children, 26 women, and 23 men average ages of 8, 7, and 6 years.
Inclusion method: Subjects in developmental age M and F, presence of flexible flat foot.
Exclusion method: Rigid flat foot, surgical treatment for flexible flat feet, presence of neurological and muscular pathologies [2,4,9].
Stabilometry: It is evaluated on subjects examined in standing position during a time of 51.2 seconds in which the patient is asked to maintain a position with the heels spaced about 1 cm and podalic alignment at 30°, with open and closed eyes, the arms are at the sides, the head straight, and a relaxed attitude.
Through this investigation, it is possible to study the attitudes that the patient implements to remedy the oscillations of the body and therefore to stabilize on the ground. The balance analysis analyzes the postural strategy used by the patient to maintain his position in a given temporal space [11,12].
The software captures the data and graphically represents the displacements on the sagittal and frontal planes of the pressure centers of the two limbs and the body’s center of gravity. Through this exam we get:
Romberg index: Description between the surface of the confidence ellipse with closed eyes and the the surface of the confidence ellipse with open eyes. It is an indicator that allows the evaluation of the contribution of the vestibular and somatosensory system to the maintenance of equilibrium (the normality values are between 65 and 220). The exam is completed by numerical values of surface and global load (of each foot) [3,12].
Therapy with vibration sound system: The name of this system (Viss) originates from the Latin “vis roboris”, that is force.
It is the evolution of the old vibrating platforms (Whole-body vibration) which, however, had two major limitations: The vibration power and the application method. These platforms were not able to produce a vibration higher than 60 Hz and could only be used in an upright position.
Humnan Tecar synergy MATT: It consists of a series of platforms that simulate differently terrains at different levels of instability with elastic thrust materials, ideal for movement with reduced joint load [13,14].
All data are given as mean ± SD. Differences between mean values before (TO) and after (TI) the rehabilitative protocol was tested for significance using Student’s test for paired observations.
The protocol involved 49 children, divided into two groups. Both groups before and after the the protocol was evaluated with a stabilometric platform. First group 29 children aged 6, 7 and 8 years, 15 female and 14 male, carried out a re-educational protocol of 10 sessions (2 per week) composed of Vibration Sound System combined with walking on Human Synergy Mat carpets [7,15].
Four Human Synergy Mat mats of different surfaces and textures were used. At the beginning of the session the child was asked to freely walk the carpets to identify the easiest and most difficult to cover to be able to fix the path to obtain an increasing difficulty for the subject [6,16,17].
Proprioceptive sensitivity is a very sophisticated mechanism that aims to provide the central nervous system with the most accurate information, in real time, about the parameters of biomechanical movement (speed, strength, direction, acceleration), physiological parameters on the state, and on the biological changes that occur in the muscles, tendons and joints as a result of the movement performed [18].
The use of these platforms is indicated in the treatment of children with flat feet because it allows them to stimulate the musculature of the plantar arch, improving gait. The materials used to allow to obtain a floating effect similar to that of a waterbed.
The platforms used in this re-educational protocol are:
Medium Density Synergy Mat, flat spurs with the elastic response of medium density, ideal for movements with the reduced joint load [8,10,13].
Hight Synergy Mat: An irregular surface that simulates the sandy soil stimulating the microcirculation and the mechanoreceptors of the foot. Activates the stabilizing musculature.
Stones Synergy Mat: Carpets of different intensities that simulate a stony and irregular surface.
It stimulates the activation of the mechanoreceptors of the sole [7,18,19,].
Subsequently, the autosomal transducers of the Vibration Sound System were applied to the affected muscles, which in the protocol of the flat foot are the gastrosoleum, anterior tibialis, peroneal and posterior tibial muscles (the transducer was not applied under the plantar vault as it would have made walking impossible.
Once the Vibration Sound System was started at a frequency of 300 Hz, the child was asked to walk back and forth on each of the carpets, in the order of difficulty established previously, for three and a half minute on each carpet for a total duration of 15 minutes [14,18,19].
During the session, we tried to educate the children about the correct step layout through tactile stimulation and verbal facilitation to carry out a greater self-correction during the execution.
VISS is a device capable of producing acoustic waves of any frequency with a sound pressure amplitude (up to 500 mbar). This device generates acoustic waves through a flow modulator and consists of two elements:
A turbine with 3200 rpm (generator) which generates a flow pressure of 250 mbar and a pressure of 500 mBar on the subject;a modulator that through a rotating system with two inputs, produces an oscillation of air with the production of sound waves with values from 50 Hz to 400 Hz. A flow modulator consists of two cylinders that rotate one inside the other and there are twelve holes per cylinder along the outer wall. The air is pumped inside the inner cylinder and when the twelve holes of the inner cylinder are aligned with the external one, the air is expelled from all the holes at the same time. Twelve tubes can be connected to the machine with as many transducers that are positioned on the affected muscles [7,10,12].
The rotation speed of the inner cylinder determines the vibration frequency. Then the turbine produces air and the modulator opens and closes the system. Autosomal transducers represent another important element of the Vibration Sound System. These can have a circular or elongated shape and can be of different sizes; in this way, depending on the body area that we intend to treat, we can use the transducer that best fits us [19,20].
Thanks to these autosomal transducers, the vibration is carried out on the person. The type of wave expressed by Vibration Sound System is a square mechanical wave capable of modifying the physical abilities of any subject, whether healthy or rehabilitating. Mechanical muscle vibration is a powerful tool for stimulating proprioceptors and is considered a useful method for clinical therapy and sports training.
The frequencies
Depending on the frequencies used, the mechanical-sound vibrations can produce different effects on the muscles. The frequencies of 50 Hz - 80 Hz have a muscle-draining effect The 120Hz frequency has a marked decrease in muscle spasticity and therefore relaxation of muscle tone. The 300 Hz frequency is used for muscle strengthening. The vibration Sound System (Viss) has long-lasting effects as it acts on the so-called “silent” mechanoreceptors that normally are not stimulated since they react too much higher frequencies (higher than 100 Hz) that our body is not able to generate [3,17,19,20].
The stimulation of these mechanoreceptors determines an impulse at the level of the central nervous system: the upper motor centers are stimulated by vibrations, to obtain a better performance of the nerve commands responsible for muscle recruitment. In this way, we do not act only at the local level (as in the case of isokinetic work and electrostimulation) but directly at the level of the nervous system producing plastic changes that last over time thanks to the long-term enhancement of selected nerve networks [6,12,13]. The activated proprioceptors are not only the neuromuscular spindles but also the Golgi tendon organs, the type III and IV mechanoreceptors and the Pacini corpuscles.
Selective vibrations have a beneficial effect on muscle metabolism, have an analgesic effect on tissues and muscle, increase local blood circulation, stimulate the formation of bone tissue and activate the secretion of specific hormones (testosterone, somatotropic hormone, and cortisol decrease). Thanks to the possibility of varying the frequency, the fields of application of Vibration Sound Systems are manifold: patients with hypotonia, or spastic hypertonia, lumbago, patients with strength deficiency, patients with incontinence, Parkinson’s and patients with a flat fee [17,19].
The mechanical-sound vibration proves to be effective in the treatment of the IV- degree flat foot because it determines: - tonification and stabilization of the cavizzanti muscles of the foot - increase in the arch of the foot -reduction of pain and fatigue - improvement of balance in an upright position optimization of postural dynamics. The second group involved 20 children aged 6, 7 and 8 years, carried out a re-educational protocol of 10 sessions (2 per week) combined with walking on carpets.
Human synergy MAT. At the beginning of the session, the child was asked to freely walk the carpets to identify the easiest and most difficult to cover to be able to fix the the path to obtaining an increasing difficulty for the subject [13,15,19,20].
Subsequently, the sitting subjects were asked to place a tennis ball in front of them. At this the point, place your foot on the ball, then move it away and bring it closer. Exercise moderate pressure downwards and rotate the ball using the entire base of the foot, up to the heel. These flat-foot exercises are designed to strengthen the arch muscles [4,7,12].
Statistical analysis
Descriptive statistics were used to describe the two groups’ characteristics. To determine if the Viss and No-Viss treatment is effective in improving physical functions, data from two different time points were analyzed: at Baseline (T0) and after... (T1). To verify if both treatments improve patients’.
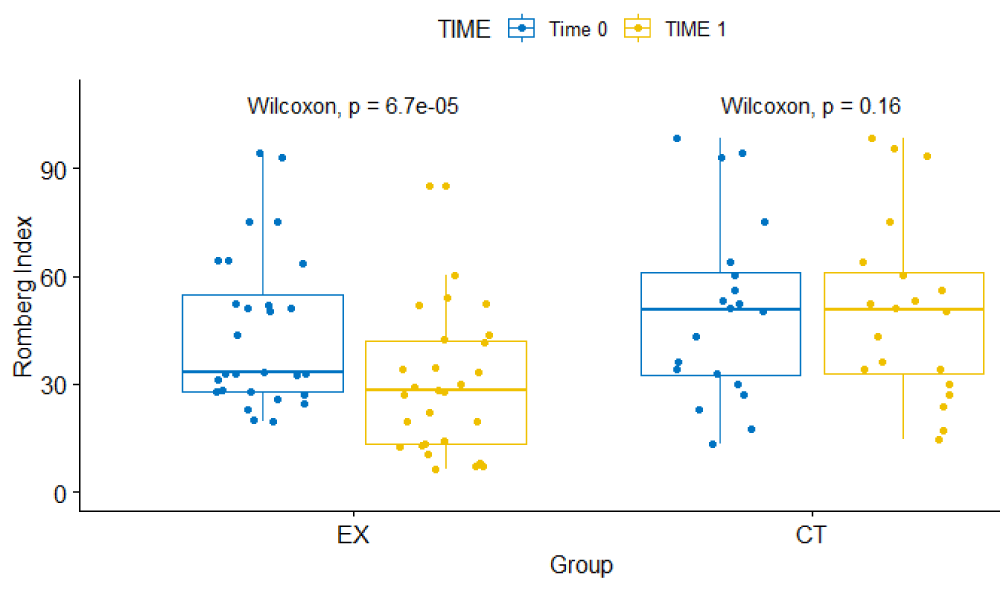
Romberg Index (IR) from T0 to T1, Wilcoxon signed-rank test were used into each group to test differences in median over time. To test if the treatment type resulted in statistically significant differences in the improvement of patient conditions, the Mann U-Whitney test was used to assess the median differences between groups before and after the treatments. The level of significance was set at p < 0.05. All tests were performed using an R statistical environment.
Table 1 displays the descriptive statistics and the non-parametric tests for non-paired (Viss vs. No-Viss group after treatments).
| Table 1: Descriptive Statistics, p-value for not-parametric between group comparisons test at Baseline (T0) and after treatments (T1). | |||
| Variable | VISS GROUP (N = 28) | NO-VISS GROUP (N = 20) | p - value |
| Median (IQR) | |||
| Age | 7.00(1.00) | 7.00(1.00) | 0.991 |
| W | 25.15(4.57) | 26.00(2.12) | 0.395 |
| Hage | 118.50(19.70) | 114.00(20.70) | 0.109 |
| BMI | 18.30(3.67) | 19.62(4.75) | 0.074 |
| CDX_T0 | 48.82(5.85) | 52.02(38.96) | 0.263 |
| CSX_T0 | 45.36(6.60) | 55.21(37.28) | 0.088 |
| CDX_T1 | 51.86(8.52) | 57.02(13.93) | 0.368 |
| CSX_T1 | 51.78(8.66) | 56.84(13.93) | 0.171 |
| Romberg Index_T0 | 33.17(27.26) | 50.70(28.82) | 0.403 |
| Romberg IndexT1 | 28.23(28.56) | 50.79(28.08) | 0.003 |
| Frequency (Row Proportion) | |||
| Sex | Male | 0.999 | |
| 13 (0.54) | 9 (0.38) | ||
| Female | |||
| 15 (0.63) | 11 (0.46) | ||
Figure 1 shows the boxplot and the Wilcoxon signed-rank test for Romberg Index (IR) in each the group over time.
Figure 1: Pairwise comparisons for Romber Index into each group at Baseline and after Treatment.
The first evidence is that the groups are in the same condition at baseline (Table 1) and they do not differ after treatment for CDX_T1 and CSX_T1 variables but differ for IR_T1. Resulting that in In the Viss group the median and iqr are 28.23(28.56) and in the No-Viss group are 50.79(28.08). In Figure 1 shows that, although among the groups the medians are different suggesting a higher value in the No-Viss group, the Romberg Index (IR) is much changed from baseline to after treatment in the group Viss while in the group No-Viss remains unchanged.
Our observational study aimed to evaluate the prevalence of flatfoot in 6-7-8 -year-olds, because it is a critical age for the development of the medial plantar arch.
In the literature, flexible flatfoot is common in most children aged under 10 years, and its incidence is approximately 45% in preschoolers and up to 15% in children of 10 years old.
Transversal epidemiological studies have shown that a flatfoot is a normal form of the foot in the first several years of life. Morley, et al. reported a prevalence of flatfoot of 97% in children aged 2 years or younger, as defined by the width ratio between the heel and medial arch [13,19].
This rate declined with age, and only 4% of 10-year-old patients had flat feet. Murray, et al. studied the direct correlation of flatfoot with joint hypermobility concerning the BS, hyperlaxity children constituted only 5% of our sample, without any statistical correlation to flatfoot. Likely, the number of study subjects with a high range in BS was too small to determine whether our data are consistent with the literature that has linked joint hypermobility and flatfoot;
We must, however, consider that the children who we screened were healthy and asymptomatic compared with those with flatfoot [15,18].
The increase in childhood obesity is one of the most serious health challenges worldwide. This the trend is a direct consequence of a sedentary lifestyle and altered eating habits.
The literature reports that individuals with flatfoot are more unstable during the upright position compared with healthy subjects.
Our results showed as a screening of plantar foot support allowed the clinicians to identify early abnormalities in plantar support at an early stage. It’s important to promptly identify the pathological flatfoot for acting with rehabilitative exercises or insoles [15,20].
Moreover, the results underline the importance of maintaining a healthy body weight for children, based on the significant correlation between overweight and flat foot. Therefore, the recognition of flatfoot is fundamental in pupils at the age of 6-7-8- years old.
- Flour F. Anatomy of the musculoskeletal system. Edises, 2008.
- Kapandji IA. Joint Physiology, Monduzzi, 2009.
- Evans AM, Rome K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur J Phys Rehabil Med. 2011 Mar;47(1):69-89. PMID: 21448121.
- HARRIS RI, BEATH T. Hypermobile flat-foot with short tendo achillis. J Bone Joint Surg Am. 1948 Jan;30A(1):116-40. PMID: 18921631.
- Staheli LT. Planovalgus foot deformity. Current status. J Am Podiatr Med Assoc. 1999 Feb;89(2):94-9. doi: 10.7547/87507315-89-2-94. PMID: 10063780.
- Uden H, Scharfbillig R, Causby R. The typically developing paediatric foot: how flat should it be? A systematic review. J Foot Ankle Res. 2017 Aug 15;10:37. doi: 10.1186/s13047-017-0218-1. PMID: 28814975; PMCID: PMC5558233.
- Orthopedics - Practical manual of orthopedics for the pediatrician Novembri, Pagliazzi, Flori, Generoso, Solito. SEE Florence 1996.
- Carr JB 2nd, Yang S, Lather LA. Pediatric Pes Planus: A State-of-the-Art Review. Pediatrics. 2016 Mar;137(3):e20151230. doi: 10.1542/peds.2015-1230. Epub 2016 Feb 17. PMID: 26908688.
- Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006 Aug;118(2):634-9. doi: 10.1542/peds.2005-2126. PMID: 16882817.
- Harris EJ, Vanore JV, Thomas JL, Kravitz SR, Mendelson SA, Mendicino RW, Silvani SH, Gassen SC; Clinical Practice Guideline Pediatric Flatfoot Panel of the American College of Foot and Ankle Surgeons. Diagnosis and treatment of pediatric flatfoot. J Foot Ankle Surg. 2004 Nov-Dec;43(6):341-73. doi: 10.1053/j.jfas.2004.09.013. PMID: 15605048.
- Re-education of the foot. Static and dynamic biomechanical and postural problems. Martinelli E. Firenze University Press 2012
- Banwell HA, Mackintosh S, Thewlis D. Foot orthoses for adults with flexible pes planus: a systematic review. J Foot Ankle Res. 2014 Apr 5;7(1):23. doi: 10.1186/1757-1146-7-23. PMID: 24708560; PMCID: PMC4108129.
- Tachdjian’s Pediatric Orthopaedics. Herring JA New York: Elsevier Saunders, 2014
- Dars S, Uden H, Banwell HA, Kumar S. The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: A systematic review: Update. PLoS One. 2018 Feb 16;13(2):e0193060. doi: 10.1371/journal.pone.0193060. PMID: 29451921; PMCID: PMC5815602.
- Benedetti MG, Ceccarelli F, Berti L, Luciani D, Catani F, Boschi M, Giannini S. Diagnosis of flexible flatfoot in children: a systematic clinical approach. Orthopedics. 2011 Jan 1;34(2):94. doi: 10.3928/01477447-20101221-04. PMID: 21323297.
- Benedetti MG. Movement analysis. Elsevier Italia S.r.l. 2005
- http://vissman.info/?page_id=165
- Pagella F, Chiappano G, Reggiani G, Di Biase D, Giuffre D, Traverso CM. Selective muscle vibrations in the treatment of neuromuscular pathologies.
- Iodice P, Bellomo RG, Migliorini M, Megna M, Saggini R. Flexible flatfoot treatment in children with mechanical sound vibration therapy. Int J Immunopathol Pharmacol. 2012 Jan-Mar;25(1 Suppl):9S-15S. doi: 10.1177/03946320120250s102. PMID: 22652156.
- https://humantecar.com/prodotti/apparecchiature/human-tecar-mat/
- Busquet L. The muscle chains. Lower limbs, Marrapese 1996.