More Information
Submitted: July 21, 2023 | Approved: July 31, 2022 | Published: August 01, 2023
How to cite this article: de Lacos LF, Blanchette A, Perreault K, Daoust R, Lee J, et al. Physiotherapy Can Help Recover Functional Status in Community-Dwelling Seniors Assessed in Emergency Departments for Minor Injuries. J Nov Physiother Rehabil. 2023; 7: 022-028.
DOI: 10.29328/journal.jnpr.1001052
Copyright License: © 2023 de Lacos LF, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Emergency department; Seniors; Injuries; Physiotherapy
Physiotherapy Can Help Recover Functional Status in Community-dwelling Seniors Assessed in Emergency Departments for Minor Injuries
Laurence Fruteau de Lacos1, Andréanne Blanchette2,3, Kadija Perreault2,3, Raoul Daoust4, Jacques Lee5, Jeffrey J Perry6,7, Marcel Émond8,9, Eddy Lang10, Nathalie Veillette11 and Marie-Josée Sirois2,9*
1Centre Intégré Universitaire de Santé et de Services Sociaux de la CapitaleNationale (CIUSSS-CN), Québec, Canada
2Département de Réadaptation, Université Laval, Québec, Canada
3Centre Interdisciplinaire de Recherche en Réadaptation et Intégration Sociale (CIRRIS), CIUSSS-CN, Québec, Canada
4Département de Médecine de Famille et Médecine d’urgence, Université de Montréal, Canada
5Department of Emergency Medicine, University of Ottawa, Canada
6Ottawa Hospital Research Institute, Ottawa, ON, Canada
7Département de médecine de famille et médecine d’urgence, Université Laval, Québec, Canada
8Centre d’Excellence sur le Vieillissement de Québec, Canada
9Cumming School of Medicine, University of Calgary. AB. Canada
10École de Réadaptation, Université de Montréal, Canada
11
*Address for Correspondence: Marie-Josée Sirois, Département de Réadaptation, Faculté de Médecine, Pavillon Ferdinand-Vandry, Bureau 3556, 1050 Avenue de la Médecine, Québec, QC G1V 0A6, Canada, Email: [email protected]
Background: Around 75% of seniors seeking treatment for injuries in Emergency Departments (ED) are discharged home with minor injuries that put them at risk of functional decline in the following months.
Objectives: To 1) describe seniors’ characteristics using or not physiotherapy services following ED visits for minor injuries and 2) examine their functional status according to physiotherapy use.
Methods: Secondary data analyses of the Canadian Emergency Team Initiative cohort study. Participants were 65 years and older, discharged home after consulting EDs for minor injuries and assessed three times: ED, 3- and 6-months. Physiotherapy use was recorded as yes/no. Functional status was measured using the Older American Resources Scale (OARS). Multivariate linear regressions were used to examine change in OARS scores over time, accounting for confounders.
Results: Among the 2169 participants, 565 (26%) received physiotherapy, and 1604 (74%) did not. Physiotherapy users were more likely females (71% vs. 64%), more educated, and less cognitively impaired. The overall change in OARS at 6 months was -0.31/28 points (95% CI: -0.55; -0.28) with no difference across groups after adjustment. Subgroup analyses among frail seniors showed that physiotherapy users maintained their function while non-users lost clinically significant function (-0.02 vs. -1.26/28 points, p = 0.03). Among the severely injured (Injury Severity Scale ≥ 5), physiotherapy users’ results were higher by almost 1/28 points (p = 0.03) compared to non-users.
Conclusion: These results suggest that among seniors discharged home after consulting the ED for minor injuries, the frail and severely injured may benefit from being systematically referred to physiotherapy services.
Community-dwelling seniors aged 65 and older sustaining minor injuries are susceptible to mobility loss and limitations in their everyday activities [1]. In Canada, a large proportion (62%) of seniors seek treatment at emergency departments (ED) following such trauma [1]. Falls are the principal cause of various minor injuries, such as contusions (14%), lacerations (9%), sprains (37%), and minor fractures (26%) [1]. As such, most of these injuries are not life-threatening, and around 75% of community-dwelling seniors are discharged back home after being assessed at EDs [2]. It has been reported that around 17% of previously independent community-dwelling seniors showed persisting functional decline six months following an ED consultation for a minor trauma [3]. The presence of gait impairments, slower walking, lower limb muscle weakness, and fear of falling, as measured during ED consult, may predict these functional losses (Sirois et al., 2015). Such physical impairments can hinder post-injury physical and social activities in injured older adults, triggering a downward spiral of decline and threatening the independence of the elderly [4,5]. Moreover, among community-dwelling seniors treated in the ED for a minor injury, frail individuals were shown to be ten times more at risk of functional decline following discharge (Sirois et al., 2015).
Global physical and functional evaluations are recommended for geriatric patients presenting to the ED after a fall [6,7]. Functional evaluations are also strongly recommended to improve physical function and health for seniors identified as frail [8]. At ED discharge, referral to targeted home-based interventions, including physical activity programs, effectively improve seniors’ functional status [7]. Unfortunately, independent older seniors with minor injuries currently receive insufficient care management services in the ED [9,10] and are released without recommended care [11,12].
Physiotherapists are experts in assessing the impact of injuries on movement and function and optimizing recovery [13,14]. Physiotherapy interventions, such as individualized exercise programs, can prevent disability and functional decline [15], decrease fear of falling, and improve gait speed in community-dwelling pre-frail seniors [16]. Newly introduced as efficient front-line providers for musculoskeletal injuries in EDs [17,18], physiotherapists are not systematically part of ED teams in Canada and rarely assess independent seniors with minor trauma.
While they may be key in preventing functional decline following minor injuries in older adults discharged from the ED, the potential impact of physiotherapy services in this population has not yet been studied.
The objectives of the present study were to 1) describe the characteristics of older adults receiving or not physiotherapy services after an ED consultation for a minor injury and 2) examine their changes in functional status in the following six months. We also explored the change in functional status between older adults receiving or not physiotherapy services among subgroups of participants.
Design
The current study is based on secondary analyses of a multi-center prospective cohort study conducted by the Canadian Emergency Team Initiative (CETI) team between March 2009 and June 2016 in Canadian teaching EDs (CHU de Quebec [Quebec City], Sacre-Coeur Hospital [Montreal], The Ottawa Hospital-Civic Campus [Ottawa], Hamilton General Hospital [Hamilton], Sunnybrook Health Sciences Center [Toronto] and Alberta Health Services [Calgary]). The main goals and results of the CETI cohort are detailed elsewhere [19]. Briefly, the CETI estimated the cumulative incidence of functional decline over six months following ED assessments of non-hospitalized injuries and identified its main determinants.
Participants
Participants were 1) aged 65 years and older, 2) seen in the ED within two weeks of a minor traumatic injury (significant soft tissue or osseous lesion that did not require hospitalization), 3) independent in 7 basic activities of daily living (BADL, described below) in the four- weeks preceding the injury, and 4) discharged home. Were excluded those who were 1) hospitalized, 2) living long-term- care facilities, or 3) were unable to give consent or communicate in French or English.
Data collection procedure
ED physicians and/or research assistants (RA) screened patients for study inclusion 24 hours a day, seven days a week. Trained RA collected data at three time points: during the ED visit (or within one week of it) and at 3- and 6-month post-ED visit. The research ethics boards of each center approved the study.
Measures
The Use of physiotherapy services was assessed through self-report at the three-time points by asking patients if they had used (yes/no) physiotherapy in the three months preceding the interview. Participants answering “yes” were assigned to the group having received physiotherapy services, while those responding “no” were assigned to the “no” group.
Functional status was measured at the three times points using the Older American Resources and Services functional scale (OARS) [20], which is validated for ED use and has good test-retest reliability [21]. The OARS assesses independence in seven basic activities of daily living (BADL: eating, grooming, dressing, transferring, walking, bathing, and continence) and seven instrumental ADLs (meal preparation, homemaking, shopping, using transportation, using the phone, managing medication and money). Each of the 14 items is scored either 0 (unable to perform without human assistance), 1 (performed with an assistive device), or 2 (completely independent). Total scores range from 0 (completely dependent) to 28 (completely independent). OARS changes of 1 or 2 points [22] are clinically significant.
Sociodemographic variables were collected at the baseline, including age, gender, and years of schooling. Social support was measured using the social support index (SSI) from the Quebec Health Surveys [23]. The SSI assesses the quantity and satisfaction of the available social support. An SSI ≥ 60.3/100 is considered good.
Injury-related variables included mechanism of injury and pain level assessed with a Visual Analog Scale (0[no pain]-10[maximum pain]) [24] as recorded by treating physicians as well as type, locations, and severity of each injury that were coded according to the 2005 revision of the Abbreviated Injury Scale (AIS) [25], in order to compute the aggregated Injury Severity Scores (ISS) which ranges from 1 (minor) to 75 (unsurvivable) [26].
Health-related variables
The number of self-reported comorbidities and general practitioner visits in the three months preceding the ED visit was recorded. The EP estimated the probability of functional decline using a 10-cm visual analog scale (0 cm = no risk; 10 cm = high risk). A 3/10 cut-off value was found to optimize the sensitivity and specificity of this variable [3]. Cognitive impairments were measured with the Montreal Cognitive Assessment (MoCA) [27] or the modified Telephone Interview for Cognitive Status (TICS-M) [28], using cut-off for impairments of 23/50 [29] and 31/50 [30], respectively.
Mobility measures included the number of falls in the previous three months, number of outings outside the home/week, frequency of use of a walking aid, walking speed (Timed Up-and-Go) [31], and fear of falling (Short Falls Efficacy scale international) [32].
Frailty status was assessed by the Canadian Study of Health and Aging-clinical frailty scale (CFS) at the ED visit [33]. It classifies older adults as very fit (level 1), well (level 2), well with treated comorbidities (level 3), apparently vulnerable (level 4) and mildly (level 5), moderately (level 6), or severely frail (level 7).
Analyses
Participants were classified into two groups based on their use of physiotherapy services within the six months following their ED visit. The baseline characteristics of participants were compared across groups using chi-square tests. The latter was also used to compare characteristics of patients lost to follow-up with those of participants.
The change in functional status between baseline and six months post-ED visit was computed for each participant. The mean changes in OARS score were first compared across groups using t-tests and univariate linear regression analyses. Multivariate linear regressions using the Least Absolute Shrinkage and Selection Operator (LASSO) method to select the models’ more appropriate co-variables among potential confounders known to have a clinical impact on functional status (age, use of a walking aid, number of outings outside the home per week, falls, baseline independence level, frailty status)[3]. Finally, using linear regressions, we explored raw changes in functional status among subgroups of participants according to frailty status, injury severity, self-reported mobility difficulty (BADL) at baseline, age, number of outings per week, and injury type. All analyses were conducted with SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Given the sample size and a significance level set at 0.05, the power to detect a difference of 1.0, 0.5, 0.3, 0.2, and 0.1 OARS points/28 between groups was 100%, 100%, 100%, 92% and 40%, respectively.
Participants
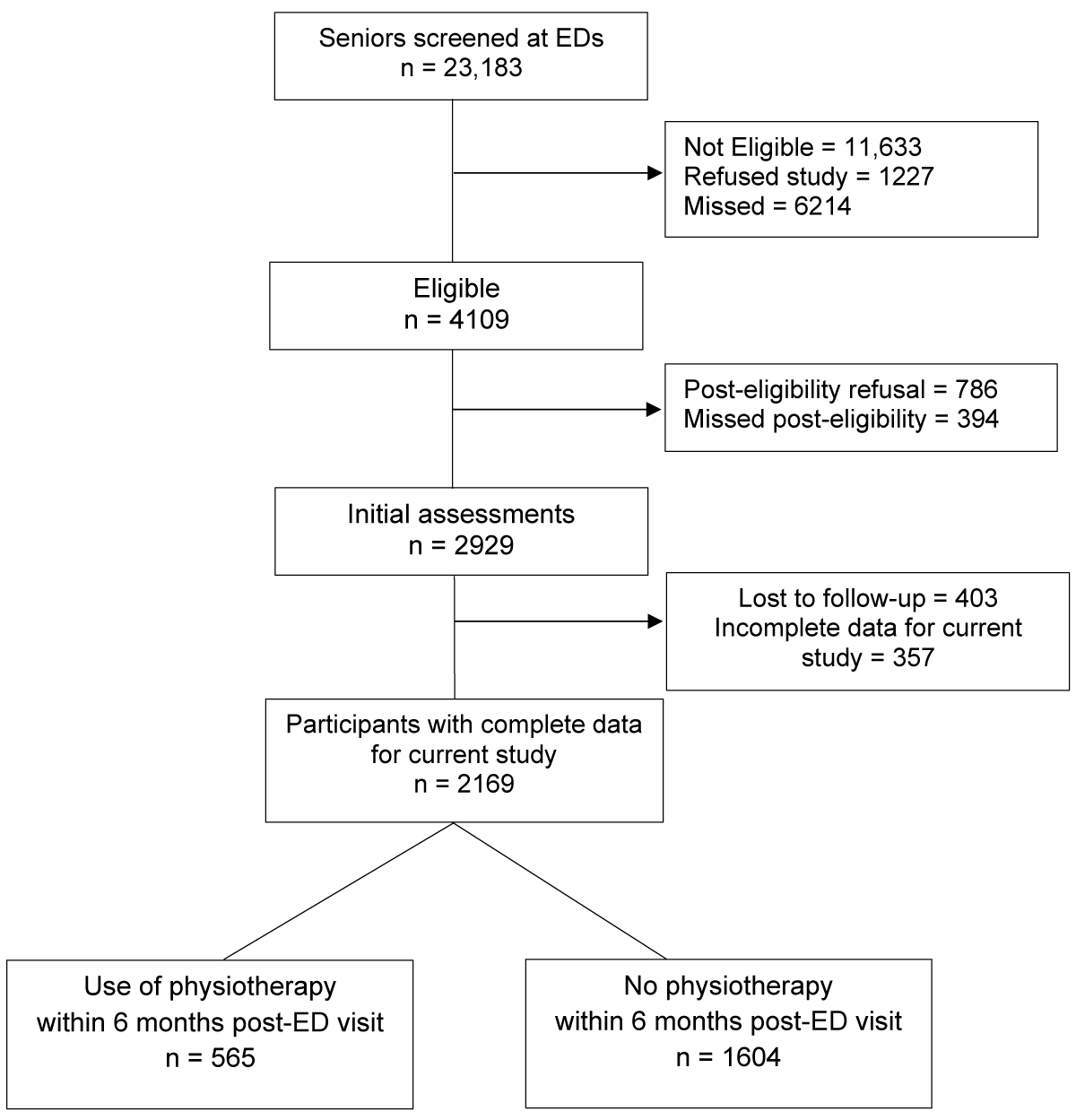
As shown in Figure 1, of the 23,183 patients screened in the EDs, 4109 were eligible, and 2929 were enrolled in the main study. There were 2169 participants with available data for the current study. Among those, 565 (26%) received physiotherapy services during follow-up, while 1604 did not.
Figure 1: Study Flow chart.
At baseline, older adults lost to follow-up had fewer comorbidities (e.g., 5 to 11: comorbidities: 32.7% vs. 38.9%, p = 0.0003) than participants. They also had more cognitive impairments (35.2% vs. 24.6%, p < 0.0001), and a higher proportion of them had under 12 years of schooling (61.8 vs. 51.5, p < 0.0001). Finally, more seniors lost to follow-up were frail (CFS=5-7/7) compared to the participants at baseline (8.1% vs. 12.4%, p = 0.006).
Table 1 describes the participants’ characteristics according to their use of physiotherapy services during the six months follow-up. Significant differences between groups were found: patients who received physiotherapy services were more likely to be female, more educated, and less cognitively impaired. A higher proportion of them were previous users of physiotherapy, were occasional users of a walking aid, and consulted the ED because of a fracture or a more severe injury. To note, patients identified as at higher risk of functional decline by ED physicians received physiotherapy services in a lower proportion following the injury (Table 1). It is also noteworthy that overall, 3% of participants were referred to physiotherapy by the treating ED physicians.
| Table 1: Baseline characteristics of community-dwelling seniors with or without physiotherapy services in the 6 months following an emergency department visit for a minor injury. | |||
| Characteristics | Physiotherapy | P - value | |
| Yes (n = 565) N (%) | No (n = 1604) N (%) | ||
| Socio-demographic | |||
| Age 65-74 | 264 (46.7) | 710 (44.3) | |
| 75-84 | 206 (36.5) | 639 (39.8) | 0.40 |
| 85+ | 95 (16.8) | 255 (15.9) | |
| Female | 420 (71.3) | 1028 (64.1) | <0.01 |
| Years of schoolingᵃ <12 (n = 2113) | 223 (40.3) | 866 (55.5) | <0.01 |
| Low social supportᵃ SSI<63 (n = 2131) | 94 (16.9) | 331 (21.0) | 0.04 |
| Health and mobility | |||
| Physiotherapist use before ED visit | 117 (20.7) | 75 (4.7) | <0.01 |
| Number of comorbiditiesᵃ (n = 2166): 0-1 | 72 (12.8) | 232 (14.5) | |
| 2-4 | 273 (48.4) | 746 (46.6) | 0.60 |
| 5-11 | 219 (38.8) | 624 (39.0) | |
| Falls in the last 3 monthsᵃ (n = 2158) | 144 (25.6) | 330 (20.7) | 0.01 |
| Less than 5 outings/weekᵃ (n = 2111) | 152 (27.7) | 468 (29.9) | 0.30 |
| Occasionnal use of a walking aidᵃ (n = 2143) | 133 (23.8) | 289 (18.2) | <0.01 |
| High pain levelᵃ (≥70/100) n = 2147 | 86 (15.4) | 240 (15.1) | 0.90 |
| Self-reported mobility difficulty (BADL) | 51 (9.0) | 90 (5.6) | <0.01 |
| Fear of fallingᵃ (FES-1≤ 9,8/10) (n = 2159) | 289 (51.4) | 771 (48.3) | 0.20 |
| Cognitive impairmentsᵃ. (n = 2070) | 108 (20.0) | 402 (26.3) | <0.01 |
| Frailty level (CFS)ᵃ (n = 1778): Robust (1-2/7) | 245 (53.6) | 668 (50.6) | |
| Pre-frail (3-4/7) | 165 (36.1) | 556 (42.1) | 0.03 |
| Frail (5-7/7) | 47 (10.3) | 96 (7.3) | |
| Risk of functional decline according to EP (≥3/10) | 449 (31.1) | 22 (43.6) | <0.01 |
| Mechanism of injury (n = 2095) | |||
| Fall | 370 (67.8) | 995 (64.2) | |
| Motor vehicle accident | 28 (5.1) | 56 (3.6) | 0.03 |
| Other | 148 (27.1) | 498 (32.1) | |
| Injury type and severity | |||
| Mild traumatic brain injury | 87 (15.7) | 301 (19.1) | 0.08 |
| Contusionsᵃ (n = 2127) | 194 (35.1) | 667 (42.4) | <0.01 |
| Lacerationsᵃ (n = 2127) | 100 (18.1) | 448 (28.5) | <0.01 |
| Sprainsᵃ (n = 2127) | 85 (15.4) | 181 (11.5) | 0.02 |
| Fracturesᵃ (n = 2127) | 228 (41.2) | 385 (24.5) | <0.01 |
| Injury severity scale (ISS, n = 1843): 1-2 | 262 (54.9) | 1010 (73.9) | |
| 3-4 | 177 (37.1) | 282 (20.6) | <0.01 |
| 5+ | 38 (8.0) | 74 (5.4) | |
| SSI: Social Support Index; ED: Emergency Department; BADL: Basic Activities of Daily Living; FES-1: Modified Falls Efficacy Scale; MOCA: Montreal Cognitive Assessment; TICS-M: Modified Telephone Cognitive Assessment; CFS: Canadian Study in Health and Aging - Clinical Frailty Scale; EP: Emergency Physician. a:Total do not fit with the total N due to missing data. |
|||
Functional status
The overall mean change in OARS scores at six months was a loss of 0.31 points (I.C. 95%: -0.55; -0.28). Table 2 describes the mean change in OARS scores across groups between initial assessments and the 6-month follow-up. The participants who received physiotherapy had a slightly lower mean OARS score throughout the study. Overall, once measures were adjusted for confounders, there were no significant differences in functional status changes across groups at the 6-month follow-up (Table 2).
| Table 2: Mean post-injury OARS scores in community-dwelling seniors with or without physiotherapy services in the 6 months following an emergency department visit for a minor injury. | |||
| Physiotherapy | |||
| Yes (n = 565) | No (n = 1604) | P - value* | |
| Mean OARS mean score (CI 95%) | |||
| Baseline 6 months |
27.0 (26.8; 27.1) 26.6 (26.4; 26.8) |
27.2 (27.2; 27.3) 26.9 (26.8; 27.1) |
< 0.01 < 0.01 |
| Mean OARS score change 0-6 months (CI 95%) | |||
| Univariate modelª Multivariate modelb |
-0.4 (-0.6; -0.2) -0.9 (-1.0; -0.7) |
-0.3 (-0.4; -0.2) -0.9 (-1.0; -0.8) |
0.24 0.60 |
| OARS: Older American Resources and Services Scale; CI: Confidence Interval. *T - tests ªResults are obtained by a linear model bResults are obtained by a linear model adjusted for confounding variables, i.e. age, fall 3 months prior to the injury, getting out of home less than 5 times /week, use of a walking aid, baseline IADL independence, and frailty status. |
|||
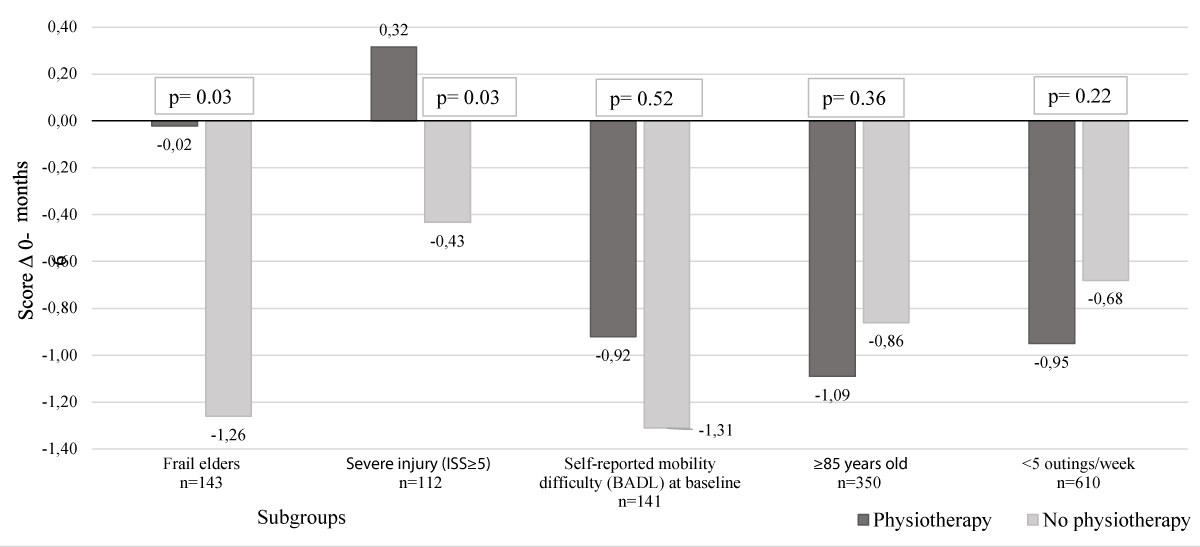
Figure 2 shows the mean OARS score change (0-6 months) according to the use of physiotherapy in subgroups of participants at higher risk of functional decline. Significant group differences were found among frail elders and participants with more severe injuries (ISS ≥5). Frail participants who did not receive physiotherapy services (n = 96) lost clinically significant OARS points, while those who received physiotherapy (n = 47) lost close to 0 points, thus maintaining a higher independence level 6 months postinjury (Figure 2). The subgroup of more severely injured participants who received physiotherapy services (n = 38) gained function (OARS points) at six months, while those who did not lost function (n = 74, Figure 2). There was no difference in OARS score change according to the use of physiotherapy among robust or less severely injured participants (ISS 1-4, data not shown). Finally, there was no difference between groups in subgroup analyses based on older age, number of outings outside the home per week, and types of injury.
Figure 2: Mean change in 0-6 months OARS score post ED visit of subgroups of participants according to exposition to physiotherapy services
This study’s primary objectives- were to describe the profile of community-dwelling older adults who received physiotherapy services vs. those who did not in the six months following an ED visit for a minor injury and to examine their changes in functional status accordingly.
This study highlighted the differences between physiotherapy receivers and non-receivers in community-dwelling seniors discharged home following a minor injury. Seniors who were fallers before the ED visit and those who had sustained fractures or needed a walking aid were more likely to receive physiotherapy services. This concurs with the general physiotherapists’ expertise in fall prevention, assistive device prescription, and progressive exercise program prescriptions following injuries [13,14,34]. The 25% of participants who received physiotherapy also had a higher education and cognitive level. Moreover, they were more frequent users of physiotherapy before the injury and had more social resources. As only 3% of participants were referred to physiotherapy by the ED physicians, this suggests that elders who felt the need for physiotherapy consultation most likely had the necessary help or resources to initiate the process themselves. Indeed, although publicly-funded physiotherapy is available under medical prescription, waiting lists are remarkably long in many Canadian provinces and can reach up to one year, even for increasingly vulnerable patients [35].
Additionally, since ED physicians scarcely prescribe physiotherapy at ED discharge for older adults with minor injuries [11,36], seniors in this study likely had to consult in private clinics at their own cost. Future studies with available data on funding sources for physiotherapy services in this older population could help better understand use patterns post-ED visits.
Whether or not participants had received physiotherapy, they tended to experience slight functional loss at six months post-ED visit. This observation is not surprising, as an important proportion of seniors from the cohort were independent and at low risk of functional decline following a minor injury [3]. Most likely for the same reason, we did not observe any difference between changes in overall functional status according to physiotherapy exposure.
However, the exploratory subgroup analyses revealed that frail and more severely injured seniors seemed to have benefited most from physiotherapy services. Frail seniors who received physiotherapy services lost less functional capacity, and the more severely injured improved their function. Those subgroups were those at higher risk of functional decline in the six months post-injury. While our subgroup analyses must be interpreted cautiously due to the smaller number of participants within subgroups, these results are consistent with existing evidence about the effectiveness of physiotherapy services for patients at risk of functional decline. Indeed, a study about hospitalized older adults reported that patients who received early physiotherapy interventions had shorter lengths of stay and returned to the community in higher proportions (Hartley et al., 2017). Comprehensive assessments in the ED by a multidisciplinary team, including physiotherapy, reduced hospital admissions, and repeated ED visits in a frail population at risk of readmission [37]. Results from a pilot study suggest the efficiency of a preventive physiotherapy program for community-dwelling older adults at high risk of becoming homebound due to functional limitations [38].
This study presents some limitations. First, we did not have information about the types of physiotherapy services received by the participants, as the CETI study was not initially designed for this specific purpose. In addition, funding sources for physiotherapy services (public or private), the content of interventions, nd treatment compliance were not documented. There was also a possible selection bias induced by the differences observed between the participants and those lost to follow-up, the latter having more frailty factors than the participants. This may limit the generalizability of our results. One main strength of this study is that it is the first to assess the relationship between exposition to physiotherapy services and functional status in previously independent, community-living seniors consulting EDs for minor injuries. Moreover, it was based on data from a large multi-center Canadian cohort representing a population that is only sparsely studied.
The results of this study suggest that among community-living seniors consulting EDs for minor injuries, frail and more severely injured individuals may benefit from being systematically referred to physiotherapy services at discharge.
- Billette JM, Janz T. Injuries in Canada: Insights from the Canadian Community Health Survey. (Catalogue no. 82-624-X). Statistics Canada. 2015. https://www150.statcan.gc.ca/n1/pub/82-624-x/2011001/article/11506eng.htm
- Canadian Institute for Health Information (2017) Emergency departments visit in Canada, Access data and reports: Quick Stats. Available at: https://www.cihi.ca/en/quick-stats
- Sirois MJ, Émond M, Ouellet MC, Perry J, Daoust R, Morin J, Dionne C, Camden S, Moore L, Allain-Boulé N. Cumulative incidence of functional decline after minor injuries in previously independent older Canadian individuals in the emergency department. J Am Geriatr Soc. 2013 Oct;61(10):1661-8. doi: 10.1111/jgs.12482. PMID: 24117285.
- Jefferis BJ, Iliffe S, Kendrick D, Kerse N, Trost S, Lennon LT, Ash S, Sartini C, Morris RW, Wannamethee SG, Whincup PH. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014 Oct 27;14:114. doi: 10.1186/1471-2318-14-114. PMID: 25348492; PMCID: PMC4223846.
- Nachreiner NM, Findorff MJ, Wyman JF, McCarthy TC. Circumstances and consequences of falls in community-dwelling older women. J Womens Health (Larchmt). 2007 Dec;16(10):1437-46. doi: 10.1089/jwh.2006.0245. PMID: 18062759.
- American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, Society for Academic Emergency Medicine, & Geriatric Emergency Department Guidelines Task Force (2014) Geriatric emergency department guidelines. Annals of Emergency Medicine 63(5): e7–e25. https://doi.org/10.1016/j.annemergmed.2014.02.008
- Hastings SN, Heflin MT. A systematic review of interventions to improve outcomes for elders discharged from the emergency department. Acad Emerg Med. 2005 Oct;12(10):978-86. doi: 10.1197/j.aem.2005.05.032. PMID: 16204142.
- Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP, Woo J, Aprahamian I, Sanford A, Lundy J, Landi F, Beilby J, Martin FC, Bauer JM, Ferrucci L, Merchant RA, Dong B, Arai H, Hoogendijk EO, Won CW, Abbatecola A, Cederholm T, Strandberg T, Gutiérrez Robledo LM, Flicker L, Bhasin S, Aubertin-Leheudre M, Bischoff-Ferrari HA, Guralnik JM, Muscedere J, Pahor M, Ruiz J, Negm AM, Reginster JY, Waters DL, Vellas B. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J Nutr Health Aging. 2019;23(9):771-787. doi: 10.1007/s12603-019-1273-z. PMID: 31641726; PMCID: PMC6800406.
- Carpenter CR, Heard K, Wilber S, Ginde AA, Stiffler K, Gerson LW, Wenger NS, Miller DK; Society for Academic Emergency Medicine (SAEM) Geriatric Task Force. Research priorities for high-quality geriatric emergency care: medication management, screening, and prevention and functional assessment. Acad Emerg Med. 2011 Jun;18(6):644-54. doi: 10.1111/j.1553-2712.2011.01092.x. PMID: 21676064; PMCID: PMC3117251.
- Tirrell G, Sri-on J, Lipsitz LA, Camargo CA Jr, Kabrhel C, Liu SW. Evaluation of older adult patients with falls in the emergency department: discordance with national guidelines. Acad Emerg Med. 2015 Apr;22(4):461-7. doi: 10.1111/acem.12634. Epub 2015 Mar 13. PMID: 25773899; PMCID: PMC6778963.
- McEwan H, Baker R, Armstrong N, Banerjee J. A qualitative study of the determinants of adherence to NICE falls guideline in managing older fallers attending an emergency department. Int J Emerg Med. 2018 Jul 18;11(1):33. doi: 10.1186/s12245-018-0192-9. PMID: 30022394; PMCID: PMC6051952.
- Miller E, Wightman E, Rumbolt K, McConnell S, Berg K, Devereaux M, Campbell F. Management of fall-related injuries in the elderly: a retrospective chart review of patients presenting to the emergency department of a community-based teaching hospital. Physiother Can. 2009 Winter;61(1):26-37. doi: 10.3138/physio.61.1.26. Epub 2009 Feb 13. PMID: 20145749; PMCID: PMC2788319.
- Canadian Physiotherapy Association (2012) Description of Physiotherapy in Canada.
- Richards S, Cristian A. The role of the physical therapist in the care of the older adult. Clin Geriatr Med. 2006 May;22(2):269-79; viii. doi: 10.1016/j.cger.2005.12.003. PMID: 16627078.
- Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Van Ness PH. A prehabilitation program for the prevention of functional decline: effect on higher-level physical function. Arch Phys Med Rehabil. 2004 Jul;85(7):1043-9. doi: 10.1016/j.apmr.2003.10.021. PMID: 15241748.
- Halvarsson A, Oddsson L, Olsson E, Farén E, Pettersson A, Ståhle A. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: a randomized controlled trial. Clin Rehabil. 2011 Nov;25(11):1021-31. doi: 10.1177/0269215511411937. Epub 2011 Aug 17. Erratum in: Clin Rehabil. 2012 Nov;26(11):1055. Oddsson, Lars [added]. PMID: 21849377.
- Desmeules F, Roy JS, MacDermid JC, Champagne F, Hinse O, Woodhouse LJ. Advanced practice physiotherapy in patients with musculoskeletal disorders: a systematic review. BMC Musculoskelet Disord. 2012 Jun 21;13:107. doi: 10.1186/1471-2474-13-107. PMID: 22716771; PMCID: PMC3599404.
- Taylor NF, Norman E, Roddy L, Tang C, Pagram A, Hearn K. Primary contact physiotherapy in emergency departments can reduce length of stay for patients with peripheral musculoskeletal injuries compared with secondary contact physiotherapy: a prospective non-randomised controlled trial. Physiotherapy. 2011 Jun;97(2):107-14. doi: 10.1016/j.physio.2010.08.011. Epub 2010 Dec 16. PMID: 21497244.
- Sirois MJ, Carmichael PH, Daoust R, Eagles D, Griffith L, Lang E, Lee J, Perry JJ, Veillette N, Émond M; Canadian Emergency Team Initiative on Mobility in Aging. Functional Decline After Nonhospitalized Injuries in Older Patients: Results From the Canadian Emergency Team Initiative Cohort in Elders. Ann Emerg Med. 2022 Aug;80(2):154-164. doi: 10.1016/j.annemergmed.2022.01.041. Epub 2022 Mar 16. PMID: 35305850.
- Fillenbaum G. Multidimensional functional assessment of older adults: The Duke Older Americans Ressources and Services procedures. Lawrence Erlbaum Associates. 1988.
- Bissett M, Cusick A, Lannin NA. Functional assessments utilized in emergency departments: a systematic review. Age Ageing. 2013. https://doi.org/10.1093/ageing/afs187
- Provencher V, Sirois MJ, Ouellet MC, Camden S, Neveu X, Allain-Boulé N, Emond M; Canadian Emergency Team Initiative on Mobility in Aging. Decline in activities of daily living after a visit to a Canadian emergency department for minor injuries in independent older adults: are frail older adults with cognitive impairment at greater risk? J Am Geriatr Soc. 2015 May;63(5):860-8. doi: 10.1111/jgs.13389. PMID: 25989564.
- Audet N, Lemieux M, Cardin J. Social and health survey 1998 - Technical and methodological notebook: Definitions and composition of the indices. Montreal, Statistical Institute of Quebec. 2001; 215 p.
- Daoust R, Beaulieu P, Manzini C, Chauny JM, Lavigne G. Estimation of pain intensity in emergency medicine: a validation study. Pain. 2008 Sep 15;138(3):565-570. doi: 10.1016/j.pain.2008.02.007. Epub 2008 Mar 24. PMID: 18359566.
- Copes WS, Champion HR, Sacco WJ, Lawnick MM, Gann DS, Gennarelli T, MacKenzie E, Schwaitzberg S. Progress in characterizing anatomic injury. J Trauma. 1990 Oct;30(10):1200-7. doi: 10.1097/00005373-199010000-00003. PMID: 2213928.
- Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988 Jan;28(1):69-77. doi: 10.1097/00005373-198801000-00010. PMID: 3123707.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005 Apr;53(4):695-9. doi: 10.1111/j.1532-5415.2005.53221.x. Erratum in: J Am Geriatr Soc. 2019 Sep;67(9):1991. PMID: 15817019.
- de Jager CA, Budge MM, Clarke R. Utility of TICS-M for the assessment of cognitive function in older adults. Int J Geriatr Psychiatry. 2003; 18(4): 318-324. https://doi.org/10.1002/gps.830
- Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology. 2011 Sep 27;77(13):1272-5. doi: 10.1212/WNL.0b013e318230208a. Epub 2011 Sep 14. PMID: 21917776.
- Knopman DS, Roberts RO, Geda YE, Pankratz VS, Christianson TJ, Petersen RC, Rocca WA. Validation of the telephone interview for cognitive status-modified in subjects with normal cognition, mild cognitive impairment, or dementia. Neuroepidemiology. 2010;34(1):34-42. doi: 10.1159/000255464. Epub 2009 Nov 5. PMID: 19893327; PMCID: PMC2857622.
- Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991 Feb;39(2):142-8. doi: 10.1111/j.1532-5415.1991.tb01616.x. PMID: 1991946..
- Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, Todd C. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008 Jan;37(1):45-50. doi: 10.1093/ageing/afm157. Epub 2007 Nov 20. PMID: 18032400.
- Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005 Aug 30;173(5):489-95. doi: 10.1503/cmaj.050051. PMID: 16129869; PMCID: PMC1188185.
- Lefmann SA, Sheppard LA. Perceptions of emergency department staff of the role of physiotherapists in the system: a qualitative investigation. Physiotherapy. 2014 Mar;100(1):86-91. doi: 10.1016/j.physio.2013.08.004. Epub 2013 Sep 27. PMID: 24268943.
- Deslauriers S, Raymond MH, Laliberté M, Lavoie A, Desmeules F, Feldman DE, Perreault K. Access to publicly funded outpatient physiotherapy services in Quebec: waiting lists and management strategies. Disabil Rehabil. 2017 Dec;39(26):2648-2656. doi: 10.1080/09638288.2016.1238967. Epub 2016 Oct 19. PMID: 27758150.
- Salter AE, Khan KM, Donaldson MG, Davis JC, Buchanan J, Abu-Laban RB, Cook WL, Lord SR, McKay HA. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporos Int. 2006;17(5):672-83. doi: 10.1007/s00198-005-0032-7. Epub 2006 Feb 21. PMID: 16491323.
- Moss JE, Flower CL, Houghton LM, Moss DL, Nielsen DA, Taylor DM. A multidisciplinary Care Coordination Team improves emergency department discharge planning practice. Med J Aust. 2002 Oct 21;177(8):435-9. doi: 10.5694/j.1326-5377.2002.tb04884.x. PMID: 12381253..
- Wilson CM, Arena SK, Adcock K, Colling D. A Home-Based Older Person Upstreaming Prevention Physical Therapy (HOP-UP-PT) Program Utilizing Community Partnership Referrals. Home Healthc Now. 2019 Mar/Apr;37(2):88-96. doi: 10.1097/NHH.0000000000000716. PMID: 30829786.
- Hartley PJ, Keevil VL, Alushi L, Charles RL, Conroy EB, Costello PM, Dixon B, Dolinska-Grzybek AM, Vajda D, Romero-Ortuno R. Earlier Physical Therapy Input Is Associated With a Reduced Length of Hospital Stay and Reduced Care Needs on Discharge in Frail Older Inpatients: An Observational Study. J Geriatr Phys Ther. 2019 Apr/Jun;42(2):E7-E14. doi: 10.1519/JPT.0000000000000134. PMID: 28628498.
- Sirois MJ, Griffith L, Perry J, Daoust R, Veillette N, Lee J, Pelletier M, Wilding L, Émond M. Measuring Frailty Can Help Emergency Departments Identify Independent Seniors at Risk of Functional Decline After Minor Injuries. J Gerontol A Biol Sci Med Sci. 2017 Jan;72(1):68-74. doi: 10.1093/gerona/glv152. Epub 2015 Sep 22. PMID: 26400735; PMCID: PMC5155653.