More Information
Submitted: June 13, 2025 | Approved: June 17, 2025 | Published: June 18, 2025
How to cite this article: Mythili G, Suganthirababu P, Selvaraj L. Systematic Review on Graded Repetitive Arm Supplementary Program (GRASP Approach) on Functional Ability of Hand, Gross and Fine Motor Control of Upper Limb in Stroke. J Nov Physiother Rehabil. 2025; 9(1): 024-029. Available from:
https://dx.doi.org/10.29328/journal.jnpr.1001067
DOI: 10.29328/journal.jnpr.1001067
Copyright license: © 2025 Mythili G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Stroke rehabilitation; Upper limb; GRASP; Motor control; Hand function; Fine motor skills; Gross motor skills
Systematic Review on Graded Repetitive Arm Supplementary Program (GRASP Approach) on Functional Ability of Hand, Gross and Fine Motor Control of Upper Limb in Stroke
Mythili G1* , Prathap Suganthirababu1
, Prathap Suganthirababu1 and Lakshana Selvaraj2
and Lakshana Selvaraj2
1Saveetha College of Physiotherapy, Saveetha Institute of Medical and Technical Science, Chennai, India
2Department of Anatomy, Sri Ramakrishna Dental College, India
*Address for Correspondence: Mythili G, PHD Scholar, Saveetha College of Physiotherapy, Saveetha Institute of Medical and Technical Science, Chennai, India, Email: [email protected]
Purpose: Stroke frequently causes severe deficits in upper limb function, which makes it difficult for patients to carry out daily tasks. An organized home-based intervention called the Graded Repetitive Arm Supplementary Program (GRASP) was developed to help stroke patients regain function in their hands and arms. This systematic review assesses the data demonstrating beneficial effects of the GRASP approach on hand function, gross and fine motor control of the upper limb in individuals post-stroke.
Methods: A systematic search was performed in databases including PubMed, Scopus, CINAHL, and Cochrane Library up to April 2025. We searched the data using Keywords such as “GRASP,” “Graded Repetitive Arm Supplementary Program,” “stroke rehabilitation,” “upper limb recovery,” “fine motor skills,” and “gross motor control.” Inclusion criteria were randomized controlled trials (RCTs), quasi-experimental studies, and cohort studies involving adult stroke survivors undergoing GRASP. Studies were excluded if they were non-English and focused on other forms of intervention. Quality assessment was performed using the PEDro scale and Cochrane risk-of-bias tool.
Results: Out of 243 studies initially screened, 8 met the inclusion criteria. Most studies reported significant improvements in upper limb function, including enhanced hand dexterity, grip strength, and coordination following participation in GRASP programs. High adherence rates and participant satisfaction were consistently noted. Some studies indicated that benefits were maintained at follow-up, suggesting long-term efficacy. Common outcome measures included the Fugl-Meyer Assessment (FMA), Box and Block Test (BBT), and Action Research Arm Test (ARAT).
Discussion: The findings suggest that GRASP is an effective adjunct to conventional stroke rehabilitation, particularly for enhancing hand function and motor control. The structured yet flexible nature of GRASP allows for scalability and adaptability to various patient needs. Limitations of the reviewed studies include small sample sizes, heterogeneity in intervention duration, and variability in outcome measures. Further research with standardized protocols and larger samples is warranted.
Conclusion: The GRASP approach appears to be a promising intervention for improving functional ability of the hand, and gross and fine motor control in the upper limbs post-stroke. Incorporating GRASP into home-based rehabilitation could enhance recovery and reduce long-term disability. Continued research is essential to establish best practices for implementation and to optimize patient outcomes
Stroke is a common neurological condition that is a leading cause of death and morbidity in both developed and low-middle-income (LMIC) nations. LMICs have a higher disease burden than high-income nations due to the 70% of strokes that occur there. Since life expectancy in India has risen to nearly 60, leading to a spike in age-related, non-communicable diseases, stroke has become the country’s fifth major cause of disability and fourth leading cause of death [1].
Any condition in which ischemia or hemorrhage affects a portion of the brain, either temporarily or permanently, and impacts one or more cerebral blood arteries is referred to as a cerebrovascular disorder [2]. Stroke is a broad term used to represent a group of illnesses with abrupt and quick onset, such as cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage [2,3]. It is one of the main causes of long-term disability and can have serious emotional and financial repercussions for patients, their families, and healthcare systems [4].
Most stroke survivors have severe arm-hand deficits and use the paretic arm and hand less frequently in daily life after a stroke. The degree of arm-hand impairment determines how the affected hand is used in day-to-day functioning, which is linked to perceived participation constraints. Additionally, a decline in health-related quality of life, limited social participation, and subjective well-being are linked to the severity of arm-hand disability [5,6].
Neurofacilitatory treatments, muscle tonus regulating therapies, progressive strengthening, biofeedback, or electrical stimulation are the current therapy approaches used for patients with severe brain injury, such as traumatic brain injury or stroke [7]. In order to improve the function of the afflicted arm, task-oriented therapies are important [8]. According to research, making the affected limb do Activities of Daily Living (ADL) tasks increases its functionality, enabling stroke patients to use their affected arm more frequently in “real-world” situations [9]. A systematic study by Kwakkel, et al. [10] also demonstrated that extended training or “augmented exercise therapy” has a positive impact on walking, dexterity, and activities of daily living in stroke patients. A therapeutic session ought to be entertaining, demanding, and inspiring. It is well accepted that motivation plays a crucial role in the effectiveness of neurorehabilitation [11].
Evidence suggests a high correlation between enhanced functional recovery and early admission to stroke units and, consequently, rehabilitation involvement. It is clear from assessments of early rehabilitation treatment for the paretic upper limb that, in contrast to facilitative techniques, repetition-based, task-oriented modalities of treatment improve motor and functional recovery. Patient inactivity during inpatient rehabilitation is a problem, even though it is known that greater therapeutic activity improves outcomes after stroke. Research conducted in both acute and subacute settings has revealed that patients engaged in therapy for 5.3% of the day, or roughly 47 minutes each day, with upper limb treatment making up only 4 to 11 minutes of that total. Furthermore, these people rest and spend alone more than 60% of the day. These results show that people could participate in therapeutic activities outside of regular therapy hours for a significant portion of the day [12].
One potential strategy to get people moving during this period is to create an exercise program that is self-administered and homework-based, in addition to treatment sessions. In order to enhance upper limb function in chronic stroke patients, self-administered exercise regimens have been effectively recommended for the home environment [12]. Intense, repetitive, and task-oriented practices are the interventions having the most evidence for accelerating upper limb recovery following a stroke [13]. Based on these evidence-based guidelines, the Graded Repetitive Arm Supplementary Program (GRASP) is a newly created self-administered intervention for the paretic upper extremity [14]. The GRASP hand program was developed by a Canadian researcher and consists of three manual exercise levels which is a graded progression of exercises including trunk control, weight bearing through the hand, repetitive bilateral arm tasks, functional strengthening exercises, range-of-motion exercises, stretching exercises and repetitive paretic arm practice [15]. A 3-point ordinal scale (0 = cannot perform, 1 = partially performs, and 2 = fully performs) is used to assign scores to each of the 33 tasks that comprise the FMA-UE (Fugl-Meyer assessment of upper extremity). The total score could be as high as 66 points or as low as 0 (hemiplegia). It assesses mobility, coordination, and reflexes in the shoulder, elbow, forearm, wrist, and hands [16]. GRASP has been widely used and was found to be beneficial in improving upper limb function and use during inpatient rehabilitation in a 2009 study. The GRASP protocol required participants to exercise for 60 minutes each day outside of scheduled therapy sessions, and they were observed by a therapist once a week. Though it requires less costly equipment and minimal increases in direct therapist time, this self-administered technique makes it affordable for all patients. The original GRASP technique used in-person sessions with a therapist to progress the exercises and track adherence. A home program might use phone monitoring to see if exercises are being completed and whether the patient is integrating their stroke-affected arm into their everyday activities. The benefits of a home-based program include the ability to more readily apply the improvements gained from repetitive exercises to everyday activities using the injured arm and hand (thereby avoiding learned non-use). Additionally, patients are being sent home early, where they might not have access to intense therapy, as hospital stays continue to decline. According to recent research, more resource-efficient interventions are needed to keep therapy going at home and/or reach patients in remote areas who might not have access to outpatient care [14].
A lot of in-office and home GRASP approach studies have been conducted to assess the recovery rate of stroke patients; therefore, this systematic review examines all English-language studies (1990–2025) evaluating GRASP in adult stroke patients, focusing on hand functional ability and gross and fine motor control outcomes. We include all study designs and outcome measures (e.g., Fugl-Meyer, Box-and-Blocks, ARAT, CAHAI, SIS, etc.) to provide a comprehensive synthesis of GRASP effects.
We conducted a comprehensive literature search (PubMed, Embase, CINAHL, Cochrane, etc.) from 1990 through 2025 for studies of post-stroke adults using GRASP. Search terms included “stroke” AND “Graded Repetitive Arm Supplementary Program” (GRASP) and related synonyms. Eligible studies were full-text English reports of any design (randomized trials, quasi-experimental, cohort, case series, etc.) testing GRASP (alone or combined with other interventions) in adults (≥ 18 years) after stroke. Outcome measures of interest were any measures of upper-limb function or use, including impairment and activity scales (e.g., Fugl-Meyer Assessment for Upper Extremity (FMA-UE), Box and Block Test (BBT), 9-Hole Peg Test (9HPT), Action Research Arm Test (ARAT), Chedoke Arm and Hand Activity Inventory (CAHAI), Stroke Impact Scale (SIS), Motor Activity Log (MAL), etc.). Two reviewers screened titles/abstracts and full texts; data were extracted on study design, sample size, intervention details (GRASP dose, setting), outcomes assessed, and results. We synthesized findings descriptively and tabulated key study characteristics and outcomes. (A PRISMA approach guided the process, although formal risk-of-bias scoring was not feasible given heterogeneity).
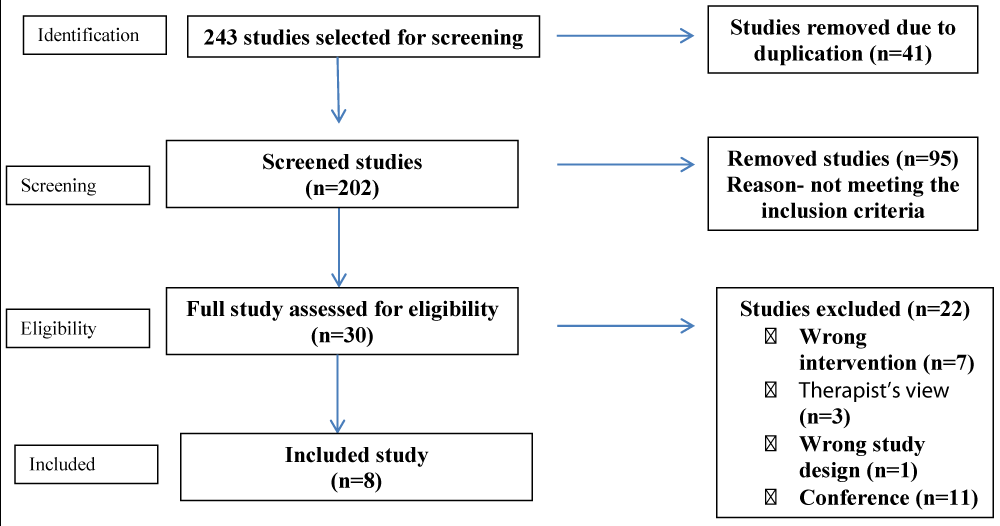
From the initial 243 studies, 235 were removed due to the duplication, overlapping of techniques, abstract not meeting the study design, wrong intervention and we included 8 studies in this systematic review [14,17,12,18-22], The results of the search are displayed explained in the PRISMA-P flow chart in Figure 1.
Figure 1: PRISMA flow diagram.
Study characteristics
We identified 8 studies with a total of 188 patients. Meeting inclusion criteria. Sample sizes per study ranged from 8 to 103 (mean ~24). The study designs included 3 randomized controlled trials, 1 pre-post pilot study, 2 mixed-methods/implementation studies, 1 cohort series, and 1 case report. Chronicity of stroke varied (acute/subacute to chronic) across studies. GRASP was delivered to the admitted patients, outpatients, or home/virtual settings, typically as a 4–8 week program (with daily practice targets of ~30–60 minutes). Seven studies used GRASP as the primary intervention, whereas one study by Wilson, et al. used standard GRASP as an active control against a virtual therapy. Outcomes were heterogeneous, but commonly included ADL-based arm function tests (CAHAI, ARAT), dexterity measures (BBT, 9HPT, MAL), strength (grip), and patient-reported function (SIS, REACH). Table 1 summarizes each study design, interventions, and findings.
| Table 1: Summary of included studies evaluating GRASP in stroke patients.Each study lists design, sample (N), intervention details (GRASP dosage, setting), outcome measures, and main results. | ||||||
| Study (Year) | Design (N) | GRASP Intervention Details | Outcome measures (key) | Main findings | ||
| Harris, et al. [12] | RCT (n = 103; GRASP = 53, Control = 50) | 4-week inpatient GRASP (self-administered exercises, ~daily) vs. education | CAHAI (primary), grip strength, paretic arm use (MAL | GRASP vs. control: Significantly greater CAHAI improvement (mean diff 6.2 points, p < 0.001); gains maintained at 5 months. Also, greater grip strength and MAL arm-use in the GRASP group. | ||
| Simpson, et al. 2017 [14] | Pre-post, pilot (n = 8; 6 completed) | 8-week home GRASP (H-GRASP), 60 min/day, phone-monitored | CAHAI, MAL (Quality of movement), grip, COPM | Baseline to post: Large effect improvements in CAHAI (Arm/Hand ADLs), MAL-Quality, grip, COPM (COPM performance/acceptability); all p ≤ 0.05. Gains sustained at 3- and 6-month follow-ups. | ||
| Arnao, et al. 2019 [17] | Pilot RCT (n = 18) | All received 4 weeks of GRASP; experimental added tRNS, control added sham tRNS |
|
GRASP+tRNS vs GRASP+Sham: Both groups improved, but the tRNS+GRASP group showed significantly greater FMA-UE gains at posttest and 1 month (p < 0.001). This pilot demonstrated feasibility and larger motor improvement with added stimulation. | ||
| Murdolo, et al. 2017 [18] | Mixed-methods pilot (n = 8) | Acute-care GRASP starting ~2–3 days post-stroke, daily during the first week | CAHAI-9, Upper Limb Motor Ability Scale (UL-MAS), SIS | Participants used GRASP ~28 min/day. Group mean changes in CAHAI-9 and UL-MAS reached clinical significance, but Wilcoxon tests did not reach statistical significance (small sample). Patients reported subjective benefits (“good for your hand,” etc). | ||
| Wilson, et al. 2021 [19] | RCT (n = 17; EDNA VR vs. GRASP control) |
|
Box and Blocks (gross dexterity), 9HPT (fine dex), SIS, NFI | EDNA vs. GRASP: EDNA group had a large, significant gain on Box-and-Blocks (g=0.90); GRASP group showed no such gross-motor gain. On 9HPT (fine dexterity), both EDNA (g=0.55) and GRASP (g=0.42) showed small improvements. No adverse events. Patient-reported SIS and caregiver NFI improved moderately in EDNA (non-significant). Overall, GRASP (control) produced only mild dexterity gains. | ||
| Yang, et al. 2021a [20] | Cohort (n = 11) – telerehab | Virtual GRASP (videoconferencing group classes) during COVID-19 (dose ~2–3×/wk) | Arm Capacity & Movement Test (ARM), SIS (Hand) | Participants showed significant improvements pre-post on both motor capacity and self-reported hand function: ARM test and SIS-Hand scores increased significantly (p < 0.05). Staff successfully delivered GRASP remotely with high adherence. | ||
| Yang, et al. 2021b [21] | Case report (n = 13) – community-based | Community center GRASP group (8-week program, twice/week sessions) | FMA-UE, ARAT, REACH (real-world arm use), SIS | After GRASP, participants had significant gains in impairment and activity: FMA-UE and ARAT scores improved, as did REACH arm-use and SIS (Hand) ratings. The program was implemented with high fidelity and adherence, improving both function and quality of life. | ||
| Levy, et al. 2021 [22] | Feasibility (n = 10) – tablet monitoring | Home GRASP (60 min/day) with electronic recording via tablet |
|
The tablet system was well accepted (mean SUS 85.5/100). Participants averaged ~50 min/day of GRASP practice (target 60 min), with self-reported ~59 min. This pilot demonstrated that home GRASP adherence can be feasibly monitored electronically. | ||
Clinical outcomes
Among all the included studies, GRASP generally produced improvements in hand and arm function. In the largest RCT conducted by Harris, et al. in 2009, GRASP yielded significantly greater gains on the CAHAI (arm/hand ADL tasks) compared to control [12]. Similarly, non-randomized studies [14] reported marked pre-post improvements in CAHAI (gross functional tasks), MAL-Quality (arm usage), and grip strength. Motor impairment (FMA-UE) also improved with GRASP use, notably in Arnao’s trial, where adding tRNS to GRASP produced larger FMA-UE increases (p < 0.001) than GRASP with sham tRNS [17]. Case reports also observed significant FMA-UE and ARAT gains post-GRASP [21].
Fine motor control
Outcomes reflecting fine dexterity generally improved with GRASP. Simpson, et al. saw significant gains in MAL-Quality (which rates fine-movement quality) [14]. A study by Wilson, et al. analysed GRASP vs. control, and the GRASP group showed a small but positive effect on the 9-Hole Peg Test (g ≈ 0.42) [19], indicating modest fine-finger dexterity gains. In Yang’s studies, virtual and community GRASP improved patient-reported hand function (SIS-Hand), suggesting better fine motor use in daily tasks [21].
Gross motor control
Measures of gross manual dexterity (e.g., Box-and-Blocks) showed mixed results. In the head-to-head trial [19], only the experimental VR group showed significant Box-and-Blocks gains, whereas the GRASP control showed none. No other included study focused on gross dexterity separately. However, gains in CAHAI and ARAT (both involving gross tasks) were noted with GRASP [12,21]. Overall, GRASP tends to improve overall arm function (including some gross tasks), but one comparative trial suggests newer technologies may yield larger gross-motor gains than standard GRASP.
Functional use and ADL
GRASP often yielded better performance in functional arm tasks and daily use. Harris, et al. (2009) found that GRASP improved the CAHAI (functional ADLs) substantially [12]. Yang, et al. [21] reported significant gains on the REACH measure (everyday arm use) and SIS self-reports [21]. The Stroke Impact Scale (hand domain) improved in most studies, and these results indicate that GRASP-related improvements transfer to perceived and real-world hand/arm function.
In summary, all included studies reported positive effects of GRASP on at least some motor outcomes. Quantitatively, controlled trials showed statistically significant group differences in arm function in favor of GRASP. Uncontrolled or feasibility studies likewise documented clinically shown improvements in muscle strength, dexterity, and task performance.
This systematic review synthesized evidence on GRASP for post-stroke arm rehabilitation. The collective findings suggest that GRASP can effectively improve upper-extremity function when delivered as an adjunct to usual care. In the largest trial, a self-administered 4-week GRASP program produced significantly greater gains in arm-hand ADL function (CAHAI) than the control group [12]. Smaller studies similarly noted improvements in arm capacity, dexterity, and strength [14,21]. Importantly, these gains persisted beyond the intervention period in at least one trial conducted by Harris, et al. with a 5-month follow-up [12].
The evidence covers multiple outcome domains. Hand functional ability (e.g., CAHAI, ARAT) consistently improved: three studies using CAHAI found increases in score with GRASP [12,18,21]. Fine motor control showed moderate gains [14,19]. Gross motor control (object-moving tasks) had less clear evidence, with only one study explicitly measuring BBT and found no GRASP effect, whereas emerging technologies had significant improvement [19]. It may be that GRASP, being largely hand/arm-focused, has its strongest impact on fine dexterity and functional tasks rather than gross strength/dexterity. Overall arm impairment (FMA-UE) improved in multiple reports, indicating the capacity of GRASP to reduce motor deficit [17,21].
Compared to other interventions, the self-directed model of GRASP is notable. It enables high-dose practice with minimal therapist time, which likely drives its benefits. The study by Simpson, et al. demonstrated the feasibility of a phone-monitored home-GRASP (H-GRASP), with high adherence (almost all patients achieved the 60-min/day target) and significant functional gains [14]. Tele-rehabilitation adaptations [19] also showed that GRASP can be delivered remotely, yielding similar motor gains [20]. These implementation studies underscore the flexibility and scalability of GRASP.
However, the evidence has limitations. Many studies were small pilot or case studies without control groups, limiting causal inferences. Only three RCTs were identified [12,17,19] – the rest were quasi-experimental or feasibility trials. Sample sizes were generally small (mean n ≈ 24) and often short-term. Outcome measures varied widely, precluding meta-analysis. A study by Wilson, et al. suggests that GRASP may be one of several effective tools, and that technology-assisted training can also be potent. Moreover, patient populations were heterogeneous (acute vs. chronic stroke, mild vs. moderate impairment), yet nearly all showed benefit.
In summary, the cumulative data indicate that GRASP exercises yield meaningful improvements in hand and arm function in stroke patients, particularly enhancing fine motor control and task performance. This aligns with rehabilitation theory: increased task-specific practice drives neuroplasticity and functional recovery. Clinicians may consider incorporating GRASP (or its variants) into stroke rehab programs to augment upper-limb therapy dose. Future research should include larger controlled trials, longer follow-ups, and comparisons with other high-intensity therapies.
The Graded Repetitive Arm Supplementary Program (GRASP) appears to be an effective upper-limb rehabilitation intervention for adult stroke survivors. Among diverse study designs, GRASP use was associated with significant gains in hand function and arm control, including improved performance on ADL-based measures (e.g., CAHAI, ARAT), enhanced fine dexterity (pegboard tasks, MAL), and better patient-reported use of the affected limb (SIS/REACH). Gross manual control showed smaller effects in one comparative trial. These findings suggest GRASP can substantially improve functional hand and arm outcomes when added to usual care, likely by increasing practice dosage. The evidence, though limited in scale, supports GRASP as a viable, low-cost adjunct for stroke rehabilitation to boost upper-limb recovery.
- Jones SP, Baqai K, Clegg A, Georgiou R, Harris C, Holland EJ, et al. Stroke in India: A systematic review of the incidence, prevalence, and case fatality. Int J Stroke. 2022;17(2):132-140. Available from: https://doi.org/10.1177/17474930211027834
- Llibre JdeJ, Valhuerdi A, Fernández O, Llibre JC, Porto R, López AM, et al. Prevalence of stroke and associated risk factors in older adults in Havana City and Matanzas provinces, Cuba. MEDICC Rev.2010;12(3):20–6. Available from: https://www.cabidigitallibrary.org/doi/pdf/10.5555/20103291205
- Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–87. Available from: https://doi.org/10.1016/s1474-4422(07)70031-5
- Shah B, Mathur P. Stroke Surveillance in India: Workshop Report. 2006 Nov. Available from: https://www.scirp.org/reference/referencespapers?referenceid=1688536
- Franck JA, Smeets RJEM, Seelen HAM. Changes in actual arm-hand use in stroke patients during and after clinical rehabilitation involving a well-defined arm-hand rehabilitation program: A prospective cohort study. PLoS ONE. 2019;14(4):e0214651. Available from: https://doi.org/10.1371/journal.pone.0214651
- Franck JA, Halfens J, Smeets R, Seelen H. Concise Arm and Hand Rehabilitation Approach in Stroke (CARAS): A practical and evidence-based framework for clinical rehabilitation management. The Open Journal of Occupational Therapy. 2015;3(4). Available from: http://dx.doi.org/10.15453/2168-6408.1164
- Langhammer B, Stanghelle JK. Bobath or motor relearning programme? A comparison of two different approaches of physiotherapy in stroke rehabilitation: a randomized controlled study. Clin Rehabil. 2000;14:361–369. Available from: https://doi.org/10.1191/0269215500cr338oa
- Michaelsen SM, Dannenbaum R, Levin MF. Task-specific training with trunk restraint on arm recovery in stroke: randomized control trial. Stroke. 2006;37:186-192. Available from: https://doi.org/10.1161/01.str.0000196940.20446.c9
- Dromerick AW, Edwards DF, Hahn M. Does the application of constraint-induced movement therapy during acute rehabilitation reduce arm impairment after ischemic stroke? Stroke. 2000;31:2984-2988. Available from: https://doi.org/10.1161/01.str.31.12.2984
- Kwakkel G, van Peppen R, Wagenaar RC, Wood Dauphinee S, Richards C, Ashburn A. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004;35:2529-2539. Available from: https://doi.org/10.1161/01.str.0000143153.76460.7d
- Liebermann DG, Buchman AS, Franks IM. Enhancement of motor rehabilitation through the use of information technologies. Clin Biomech. 2006;21:8–20. Available from: https://doi.org/10.1016/j.clinbiomech.2005.08.006
- Harris JE, Eng JJ, Miller WC, Dawson AS. A self-administered Graded Repetitive Arm Supplementary Program (GRASP) improves arm function during inpatient stroke rehabilitation: a multi-site randomized controlled trial. Stroke. 2009;40(6):2123-8. Available from: https://doi.org/10.1161/strokeaha.108.544585
- Veerbeek JM, van Wegen E, van Peppen R, van der Wees PJ, Hendriks E, Quinn TJ, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS One. 2014;9:e87987. Available from: https://doi.org/10.1371/journal.pone.0087987
- Simpson LA, Eng JJ, Chan M. H-GRASP: the feasibility of an upper limb home exercise program monitored by phone for individuals post stroke. Disabil Rehabil. 2017;39(9):874-882. Available from: https://doi.org/10.3109/09638288.2016.1162853
- Connell LA, Mcmahon NE, Watkins LA, Eng JJ. Use of the Graded Repetitive Arm Supplementary Program (GRASP) intervention: a practice implementation survey study. Phys Ther. 2014;94(5):632-643. Available from: https://doi.org/10.2522/ptj.20130240
- Lundquist CB, Maribo T. The Fugl–Meyer assessment of the upper extremity: reliability, responsiveness and validity of the Danish version. Disabil Rehabil. 2017;39(9):934-939. Available from: https://doi.org/10.3109/09638288.2016.1163422
- Arnao V, Riolo M, Carduccio F, Tuttolomondo A, D'Amelio M, Brighina F, et al. Effects of transcranial random noise stimulation combined with Graded Repetitive Arm Supplementary Program (GRASP) on motor rehabilitation of the upper limb in sub-acute ischemic patients: a randomized pilot study. J Neural Transm. 2019;126(12):1701–6. Available from: https://doi.org/10.1007/s00702-019-02087-9
- Murdolo Y, Brown T, Fielding L, Elliott S, Castles E. Stroke survivors’ experiences of using the Graded Repetitive Arm Supplementary Program (GRASP) in an Australian acute hospital setting: a mixed-methods pilot study. Aust Occup Ther J. 2017;64:305–13. Available from: https://doi.org/10.1111/1440-1630.12363
- Wilson PH, Rogers JM, Vogel K, Steenbergen B, McGuckian TB, Duckworth J. Home-based (virtual) rehabilitation improves motor and cognition function for stroke patients: a randomized controlled trial of the Elements (EDNA-22) system. J Neuroeng Rehabil. 2021;18(1):165. Available from: https://doi.org/10.1186/s12984-021-00956-7
- Yang C-L, Waterson S, Eng JJ. Implementation and evaluation of the virtual Graded Repetitive Arm Supplementary Program (GRASP) for individuals with stroke during COVID-19 pandemic and beyond. Phys Therapy. 2021;101(6):pzab083. Available from: https://doi.org/10.1093/ptj/pzab083
- Yang C-L, Bird ML, Eng JJ. Implementation and evaluation of the Graded Repetitive Arm Supplementary Program (GRASP) for people with stroke in a real-world community setting: case report. Phys Therapy. 2021;101:pzab008. Available from: https://doi.org/10.1093/ptj/pzab008
- Levy T, Killington M, Lannin N, Crotty M. Viability of using a computer tablet to monitor an upper limb home exercise program in stroke. Physiother Theory Pract. 2021;37(2):331–41. Available from: https://doi.org/10.1080/09593985.2019.1625092