Table of Contents
Rehabilitation of hearing by cochlear implantation
Published on: 24th July, 2019
OCLC Number/Unique Identifier: 8206594527
Background: Cochlear implants (CI) are nowadays a widely accepted treatment for sensorineural hearing loss SNHL.
Aim: This study aimed to describe the epidemiological characteristics and the surgical approach and to evaluate the outcomes of our experience in cochlear implantation.
Setting: Department of Otolaryngology-Head and Neck Surgery of University Hospital Mohammed VI Marrakech Morocco.
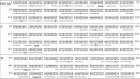
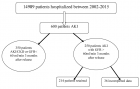
Methods: A retrospective chart review was conducted on 113 patients with severe to profound hearing loss who underwent a cochlear implantation between 2007-2018.
Results: There were 65 females and 48 males with severe to profound bilateral deafness, of whom 103 had prelingual deafness. The mean age of pediatric cochlear implantation was 5.25 years. Implantation was unilateral in all patients. The procedure was followed by regular adjustments and speech therapy. The evaluation was carried out by the same team each month during the first 6 months, then every 6 months. The average duration of follow-up was 37.54 months. All patients benefited from their implants with inter individual variability.
The good results were correlated with early implantation, significant parental investment and a steady follow-up of speech therapy.
Conclusion: Cochlear implantation has revolutionized the management of severe to profound deafness. It is a safe and effective technique when it is aimed at correctly selected populations.
Postural and Kynematic effect of a new custom-made foot insole called “Prodynamic” in a cohort of patients affected by extrapiramidal disease
Published on: 23rd May, 2019
OCLC Number/Unique Identifier: 8164054497
Background: The use of a custom-made orthotic plantar device is referenced as a true sensor-motor facilitation tool for the control of the postural orthostatic and orthodynamic position in patients with Parkinson’s disease.
Aim: To outline the postural and kinematic effect of a pro-ergonomic multilayer foot insole versus a custom-made carbon-kevlar dynamic foot insole in a cohort of patients affected by extrapyramidal disease.
Setting: A rehabilitation institute for the treatment of neurological and orthopaedic gait disorders.
Methods: A sample of 8 patients (mean age of 82.6), of whom 4 affected by Parkinson’s disease (P) and 4 by Parkinsonism (PS) were recruited for the aim of this study. In line with our inclusion criteria (clinical-functional diagnosis of Parkinson’s disease or Parkinsonism, Webster scale ≤ 20, Mini-mental State Examination (MMSE) ≥ 18), the study design developed in 2 times:
a. time T1 (or evaluation time), in which recruited patients affected by Parkinson’s disease or Parkinsonism were evaluated at the Hospital and Noble Resting House Paolo Richiedei through an accurate functional (Conley scale, Barthel Index scale, Tinetti scale and the Berg Balance Scale), postural evaluation (VPA) and walking examination (VGA, baropodometric evaluation, kinematic gait evaluation through WIVA system); to each group of patients of our study were therefore entrusted 4 foot-insoles, of which 2 synthetic and 2 carbon-kevlar custom-made foot-insoles called PRODYNAMIC; at the end of this step, patients started with our integrated rehabilitative treatment course.
b. time T2 (or experimental time; 90 days from T1), a new clinical-instrumental evaluation of each patient was performed, repeating the clinical-functional and instrumental evaluation performed at the time T1 in a specular way; this assessment was performed in FW condition, with personal footwear and previously acquired foot-insoles used during the evaluation at the T1 time.
Results: Most of our patients have been able to find benefit from the use of the plantar orthosis and integrated rehabilitation treatment so as to bring some modifications within personal postural attitude, recording an improvement but not uniform change within the sample. The results obtained by comparing the VPA at time T1 and at time T2 explain how patients affected by both clinical forms tend to establish incorrect postural attitudes due to stiffness and appearance of hypertonic plasticity, which become then structured and only partially modifiable. There was a general performance improvement in line with the VGA: within the P.B group, we observed with the use of the Prodynamic insole a partial or even complete normalization of the dynamic heel-contact phase, a better alignment of the COP in its excursion from the 1st to the 2nd rocker phase of the step, a notable facilitation to the inertial thrust in progress in the 3rd and 4th rocker phase, an improvement in the eccentric control of the patellofemoral alignment in the acceptance phase of the so-called load-response in stance and, finally, the acquisition of a more physiological propulsion structure of the trunk basin unit with an improvement of the clearance and fixation skills in the sequential phases of the step. This trend was evident but not uniform in the other groups considered. Analysis of the evolution of the degree of functionality in the daily life activities expressed by the Barthel index, passing from time T1 to the time T2, showed an improvement and consistent change in all groups considered within our study that we can find in a more or less way for the other clinical outcome data. An objective time-related and intra-group comparison of the raw static and dynamic baropodometric data acquired in our 4 study conditions showed different time-related trends for the two groups taken into consideration. A specific WIVA profile was found for each pathology group, highlighting different trends passing from time T1 to time T2 in particular of the gait cadence and gait speed. In particular, in the “Prodynamic” study condition the gait cadence shows in the Parkinson group a significant increase from time T1 to time T2, passing respectively from an average value of 41.9 ± 11.7 to 54.9 ± 1.1; patients of the Parkinsonism group showed a value of the average gait cadence at time T1 higher than the other study conditions at the same evaluation time, with an increase of this data from T1 to T2, passing from 43.1 ± 11.8 to 47.4 ± 4.4. If we consider the gait speed time-related trend, in the “Prodynamic” study condition at T1 the gait speed in Parkinson patients is similar to that recorded in the “shoe” study condition; in Parkinsonism the gait speed recorded at time T1 is higher than that recorded in the other study conditions; at time T2 there is a less evident increase in speed compared to that observed in patients with Parkinson’s.
Conclusion: In today’s management of the profile of complexity of extrapyramidal pathology, the association of several health figures is of fundamental importance, with professional profiles and diversified skills, in such a way as to be able to guarantee a comprehensive management of the patient. From this point of view, the figure of the orthopedic technician will be able to play a new role within the rehabilitation team, which will be responsible for the best possible functional response (deriving from an optimal integration between orthotic and rehabilitation treatment) of patients with Parkinson’s disease.
Kinesio taping in patients with shoulder impingement
Published on: 22nd May, 2019
OCLC Number/Unique Identifier: 8163920703
Study Design: Prospective Observational Study.
Background: Physical therapy is one of the primary treatment options for these patients, however, we were unable to identify previously published research that objectively assesses the impact of taping on joint range of motion or on pain levels in patients with SAIS. This gap in the literature motivated the present study.
Objectives: To describe the results of the application of neuromuscular taping in patients with subacromial impingement syndrome (SAIS), with respect to their pain levels, joint range of motion, and acromiohumeral distance, assessed via ultrasound.
Methods: A prospective series of cases was evaluated at the Hospital Italiano de Buenos Aires between April and September of 2018. Twenty-four patients from age 25 to 65 were invited to participate (9 men and 15 women), all of whom had been diagnosed with rotator cuff tendinopathy, impingement syndrome, or bursitis with positive signs of impingement in the affected shoulder and anterior shoulder pain in flexion.
Result: Significant changes in AHD (Figure 2), pain, and anterior flexion were registered after taping. Superficial dermatitis was detected in only two patients, but this did not affect the assessment.
Conclusion: In the results obtained by this study, it has been observed that the application of neuromuscular taping using the method described above significantly increases AHD, leading to short-term improvements in pain and joint range of motion.

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."